Vascular Surgery
VASCULAR SURGEONS AT THE SURGICAL CLINIC

Dr. Thomas Beazley
Vascular Surgeon
VIEW PROFILE

Dr. Julia Boll
Vascular Surgeon
VIEW PROFILE

Dr. JimBob Faulk
Vascular Surgeon
VIEW PROFILE

Dr. Brian Kendrick
Vascular Surgeon
VIEW PROFILE

Dr. Billy J. Kim
Vascular Surgeon
VIEW PROFILE

Dr. Allen Lee
Vascular Surgeon
VIEW PROFILE

Dr. Caroline Nally
Vascular Surgeon
VIEW PROFILE

Dr. Elizabeth F. Nelson
Vascular Surgeon
VIEW PROFILE

Dr. Adam Richter
Vascular Surgeon
VIEW PROFILE

Dr. Mark Shelton
Vascular Surgeon
VIEW PROFILE

Dr. Todd H. Wilkens
Vascular Surgery
VIEW PROFILE

Dr. Patrick Yu
Vascular Surgeon
VIEW PROFILE
Vascular conditions we treat
Aortic aneurysm
Abdominal aortic aneurysms (AAA) is a bulge in the blood vessel that runs from the heart to through the abdomen. If not spotted early and repaired, an aneurysm can rupture and cause life-threatening internal bleeding. At The Surgical Clinic, our surgeons offer several surgical options for treating AAA.
Carotid artery disease
A condition involving the narrowing of the arteries leading from the heart to the brain. Causes include the build-up of cholesterol and fat (atherosclerosis) and blood clots. If left untreated, this condition could cause strokes or brain damage. At The Surgical Clinic, we offer testing, diagnosis, and surgery for the treatment of carotid artery disease.
Deep vein thrombosis (DVT)
A deep vein thrombosis (DVT) is a blood clot in a large vein deep inside a leg, arm, or another part of the body. DVT often causes circulation problems, venous ulcers, varicose veins, spider veins, and edema. Additionally, DVT can separate from the vein and travel to the lungs–causing a pulmonary embolism (PE). The clot in the lungs can cut off the flow of blood. If this occurs, it is a medical emergency and may cause death.
Dialysis access management
Dialysis access is used to treat kidney disease and end-stage renal disease (ESRD). Dialysis treatments are often needed multiple times per week, so having a healthy dialysis access port created and maintained is essential for dialysis patients.
Mesenteric disease
Mesenteric vascular disease is a condition that develops when the arteries in the abdomen that supply the intestines with blood become narrowed due to the build-up of plaque (a process called atherosclerosis). The result is a lack of blood supply to the intestines (UMCVC). Symptoms of this disease include unexplained weight loss and pain that occurs after eating.
Peripheral artery disease (PAD)
Peripheral arterial disease is a condition that develops with age and can be made worse due to smoking, high cholesterol, and plaque build-up in the arteries. All of these factors make it more difficult for your blood vessels to healthily carry your blood through your body. PAD is also often connected to other vascular diseases like carotid artery disease, DVT, strokes, and varicose veins.
Spider & Varicose Veins
Spider veins and varicose veins are two sides of the same coin. Alone, neither are a serious medical problem. However, varicose veins especially can lead to swelling, pain, and heaviness in your limbs. Our vascular surgeons at The Surgical Clinic offer many treatments to help you manage and resolve your varicose and spider vein problems.
Vein Stripping
Vein stripping is a surgical treatment for varicose veins that involves removing the saphenous vein—the main vein in your leg that often contributes to bulging, uncomfortable veins. Typically performed in a hospital setting, this procedure is designed to relieve symptoms and improve blood flow in the affected limb.
After vein stripping, most patients notice some bruising and swelling for the first couple of weeks. Wearing compression stockings is recommended during this period to aid healing and minimize discomfort. Light walking is encouraged soon after surgery to support circulation, but it’s best to avoid strenuous activities while you recover. Most people are able to return to work or their usual daily routines within 1 to 2 weeks, with a full return to normal activities generally expected in about 2 to 4 weeks.
Thoracic Outlet Syndrome
Thoracic outlet syndrome is a set of symptoms in the shoulder, arm, or hand. It occurs from a narrowing of the thoracic outlet. This is the space between your collarbone and your first rib. It can result from injury, disease, or a problem present from birth. Thoracic outlet syndrome is not common, but it can occur in people of any age. It usually causes pain and numbness in your shoulder, arms, hands, and fingers.
Vascular procedures & treatments
Abdominal Aortic Aneurysm Surgery (AAA)
Amputation Lower Extremity
Aneurysm Repair
Angioplasty and Stenting
Aortobifemoral Surgery
Arteriogram
Awake Carotid Endarterectomy
Dialysis Access Surgery
Dialysis Catheter Insertion/Removal
Dialysis Shunt Insertion/Removal
Endovascular Abdominal Aortic Aneurysm Repair (EVAR)
Endovascular Intervention
Endovascular Thoracic Aortic Aneurysm Repair (TEVAR)
Endovenous Laser Ablation
Hybrid Aortic Aneurysm Repair
IVC filter placement/removal
Limb Salvage
Lower Extremity Amputation
May-Thurner Syndrome
Mesenteric Aneurysms and Occlusive Disease
Pelvic Congestion
Peripheral Artery Bypass for PAD
Phlebectomy of Varicose Veins
Port-A-Cath Insertion/Removal
Radiofrequency Ablation
Reflux Vein Closure
Revascularization Surgery
Sclerotherapy
Spider Vein Treatment
Thoracic Debranching for Arch Aneurysmal Disease
Thoracoabdominal Aneurysm Repair
Transcarotid Artery Revascularization (TCAR)
Treatment of Deep Venous Thrombosis
Upper Extremity Endovascular
Varicose Vein Treatment
Vascular Surgery
Venous Disease
Venous Stent
Wound Care
Vascular Surgery in Nashville
Your body is fed by a network of arteries and veins.
Arteries are large tubes that let blood travel away from your heart, with the exception of the pulmonary artery. This blood is filled with oxygen and nutrients, the fuel source for your entire body. Blood circulates throughout the body, delivering fuel and collecting its waste products, such as carbon dioxide.
Veins are smaller than arteries, and they carry blood back to your lungs. Here, the blood is refilled with oxygen. Then, it is shipped to your heart and finally pumped back out again. A single droplet of blood will make this complete tour of your body every minute.
In order to work properly, arteries and veins have to be elastic enough to withstand the pressure of blood pumping. But they also can’t become saggy, or blood will accumulate in your extremities and not properly return to your lungs.
You will need surgery if veins or arteries have stretched, developed weak spots, clogged, or lost their elasticity. Surgery will eliminate or circumvent the diseased area.
In areas outside the intracranial and coronary arteries, specialized vein surgeons will surgically treat arterial, venous, and lymphatic system conditions. Some vascular conditions will occur only in arteries, while others occur only in veins. There are some disease processes that will affect both arteries and veins.
Vascular Surgeons
in Nashville Area
Julia (Julie) Boll, MD, RPVI
JimBob Faulk, MD, FACS, RPVI
Dr. Brian Kendrick, MD
Billy J. Kim, MD, FACS
Allen P. Lee, MD, FACS, RPVI
M. Caroline Nally, MD
Elizabeth F. Nelson, MD, RPVI
Adam A. Richter, MD, FACS, RPVI
Mark W. Shelton, MD
Dr. Todd Wilkens, MD
Dr. Patrick Yu, MD
Vascular & Vein Treatments
Vascular and Vein treatments in Nashville
Your first appointment with a vascular surgeon will involve a vascular ultrasound.
This test will help the trained vascular specialist assess the condition of your veins.
Ultrasounds also help your surgeon know the exact position of your veins to plan a more effective course of treatments. If serious intervention is necessary, we can talk you through vascular surgery options.
Peripheral Artery Disease (PAD)
Peripheral artery disease (PAD) is a vascular condition characterized by narrowed arteries that reduce blood flow to the limbs, most commonly the legs. This narrowing is often caused by atherosclerosis, a buildup of plaque in the arterial walls. PAD can lead to symptoms such as leg pain, cramping, numbness, or weakness, particularly during physical activity. Left untreated, PAD can progress to more severe complications, including non-healing wounds, tissue damage, and even limb amputation in extreme cases. Diagnosis typically involves a combination of medical history review, physical examination, and non-invasive tests such as ankle-brachial index (ABI) measurement or Doppler ultrasound. Treatment strategies for PAD aim to alleviate symptoms, improve circulation, and reduce the risk of complications. Lifestyle modifications such as smoking cessation, regular exercise, and a healthy diet are essential components of PAD management. Additionally, medications to manage cholesterol, blood pressure, and blood sugar levels may be prescribed. In advanced cases or when symptoms are severe, minimally invasive procedures such as angioplasty or bypass surgery may be recommended to restore blood flow to the affected limbs. Early detection and proactive management are crucial in preventing progression and optimizing vascular health for individuals living with PAD.
What to Expect After Vein Stripping
Recovery from vein stripping, a procedure often used to treat troublesome varicose veins in the leg, typically unfolds over the course of a few weeks. You can expect some bruising and swelling in the treated leg for the first couple of weeks, which is a normal part of the healing process. Wearing compression stockings as recommended can help minimize these symptoms and support healthy blood flow as your body recovers.
It’s important to get up and walk soon after the procedure—gentle activity helps promote circulation and speeds up healing. Begin with light walking and gradually increase your activity level as you feel comfortable, taking care to avoid intense or strenuous exercise in the early stages. Most people find they can return to regular work activities within one to two weeks, while a full recovery generally takes two to four weeks.
If you experience significant discomfort, elevating your legs and using over-the-counter pain relief can help manage mild symptoms. Always follow your surgeon’s advice for wound care and activity, and reach out to them if you notice unusual swelling, pain, or signs of infection.
Physical Activity After Vein Procedures
Following a vein procedure, gentle walking is encouraged as soon as you feel able. Light activity helps promote healthy blood flow and reduces the risk of complications. Most patients can gradually return to their everyday routines over the first couple of weeks. However, you’ll want to avoid strenuous activities—especially running, jumping, or heavy lifting—during this initial healing period. A good rule of thumb: ease back into your usual schedule, listening to your body and skipping high-impact workouts until cleared by your surgeon.
Recovery After Office-Based Vein Procedures
When it comes to office-based treatments like sclerotherapy and endovascular vein therapy, the recovery process tends to be straightforward and manageable for most people. Typically, recovery time for these procedures ranges from about one to two weeks. During this period, it’s common to experience some bruising and swelling—nothing out of the ordinary, and these symptoms usually improve with the use of compression stockings, which you’ll wear for the first week or two.
One of the advantages of these minimally invasive therapies is how quickly you can return to daily routines. Most patients are able to go back to work as soon as the next day following their procedure. Light walking is encouraged right away, helping to promote healthy circulation and speed healing. However, it’s best to avoid activities that involve running or jumping for the first two weeks, giving your veins a chance to heal properly.
Overall, with a little care and some minor adjustments to your activity, recovery after sclerotherapy or endovascular therapy is typically smooth and allows for a quick return to normal life.
Returning to Work After Vein Procedures
Many patients wonder how soon they’ll be able to get back to work after a vein procedure. Fortunately, most modern treatments are designed with minimal downtime in mind.
For minimally invasive procedures—such as sclerotherapy or endovascular vein therapies for varicose and spider veins—recovery is generally quite fast. In most cases, patients are able to resume desk jobs or light activities as soon as the following day. Mild bruising and swelling are expected, but wearing compression stockings for one to two weeks can help alleviate these symptoms. Gentle walking is encouraged right after your procedure, but you should hold off on running or high-impact activities for about two weeks.
For surgical vein stripping, which is less common but sometimes necessary for more significant vein issues, recovery takes a bit longer. Patients will typically notice swelling and bruising for a couple of weeks and are also advised to use compression stockings during this period. Most people can expect to return to work within one to two weeks after surgery, though full recovery may take up to a month. Again, staying lightly active—like walking—is recommended to boost circulation, but strenuous exercise should be postponed until your surgeon gives the all-clear.
What to Expect After Vein Procedures
It’s completely normal to experience some bruising and swelling following vein treatments. These effects are a natural part of the healing process as your body adjusts. To minimize discomfort and speed up recovery, your surgeon will likely recommend wearing compression stockings for the first week or two. These specialized stockings help support your veins, reduce swelling, and encourage healthy blood flow during your recovery period.
If you have concerns about sensations or noticeable changes after your procedure, be sure to reach out to your care team—they’re here to make your recovery as smooth as possible.
What is vascular surgery?
Vascular surgery is a specialty surgery practice used to manage heart and blood flow problems. These issues include vascular infections and vascular diseases, which affect the vascular system, veins, arteries, and lymphatic circulation. Some conditions that vascular surgeons treat include Peripheral Artery Disease, Chronic Venous Insufficiency, Deep Vein Thrombosis, atherosclerosis, and aneurysms.
Minimally invasive surgeries like catheter procedures and surgical reconstruction are utilized in vascular surgery medical therapies.
Only a trained surgeon, called a vascular surgeon, can treat vascular problems and diseases. People sometimes also call these specialists an artery surgeon or blood vessel surgeon, since they treat arterial and blood vessel problems.
Common vascular surgery techniques include:
→ Atherectomy – removal of atheroscolerosis, or surgical removal of plaque build up from blood vessels
→ Angioplasty and stenting – procedure to widen narrowed or blocked arteries or veins
→ Arteriovenous (AV) fistula – surgical connection between an artery and a vein
→ Arteriovenous (AV) graft – similar to AV fistula, but a surgeon will connect an artery to a vein with a synthetic tube
→ Thrombectomy – procedure to remove a blood clot from an artery or vein
→ Open abdominal surgery – for abdominal aortic aneurysm repair
→ Vascular bypass surgery – procedure to reroute blood flow to pass a blocked artery, commonly a vascular surgery performed on legs
→ Open carotid and femoral endarterectomy – surgical removal of plaque from arteries that run from the neck to the brain (carotid), or plaque removal from arteries running from groin to legs (femoral)
Recovery After Arterial Procedures: Balloon Angioplasty and Stenting
After undergoing arterial procedures like balloon angioplasty and stenting, patients typically spend a short period in the hospital for monitoring and initial recovery. Mild bruising or soreness near the procedure site is common in the first few days, but these symptoms generally resolve on their own.
During recovery, patients are encouraged to begin walking soon after the procedure, gradually increasing their activity as they feel more comfortable. However, it’s important to avoid sitting or standing for extended periods. When resting, elevating the legs can help promote healthy circulation and reduce swelling.
Full recovery usually takes around eight weeks, though this can vary depending on individual health and the complexity of the procedure. Following your care team’s instructions—regarding activity restrictions, medications, and wound care—will help ensure a smooth healing process and improve long-term vascular health.
What is a VPC?
Vascular Procecdure Center (VPC) → Learn about our Vascular Procedure Center where we perform venous and vascular procedures for our patients across Tennessee. Using the latest minimally invasive surgical techniques, we offer patients hospital-level care in a convenient outpatient facility.
As an independent procedure center in the Nashville area, we have access to the most cutting-edge vascular procedure techniques and technologies. These techniques and technologies are not available anywhere else.
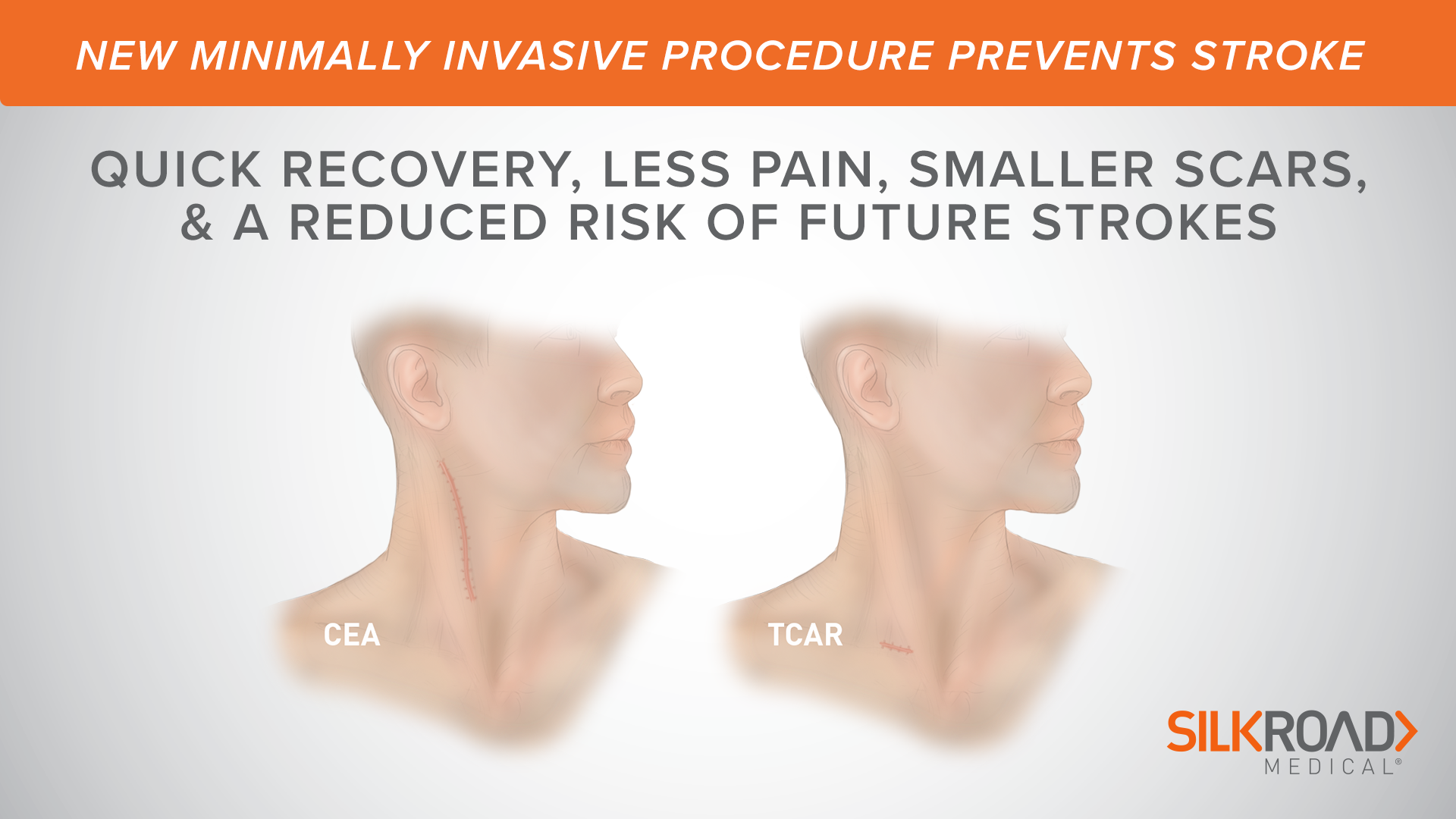
TCAR Procedure
Transcarotid Artery Disease Treatment
What is TCAR?
TCAR stands for transcarotid artery revascularization. This procedure is a minimally invasive option for carotid artery disease compared to traditional options like CEA (carotid endarterectomy). By taking a less invasive approach, we’re able to help mitigate risks associated with traditional surgery.
Abdominal Aortic Aneurysm
Vascular Surgery: Aortic Aneurysms
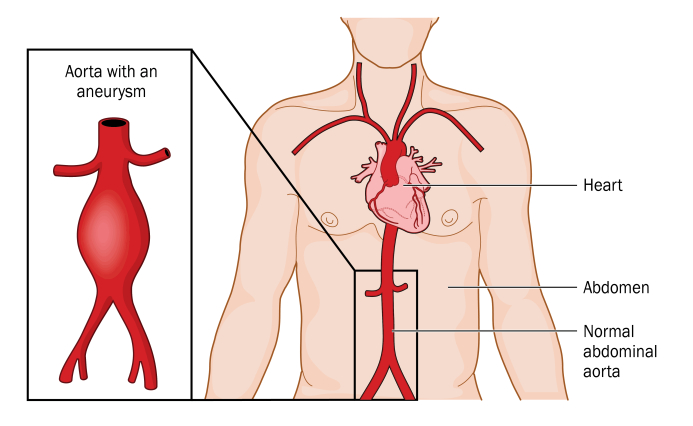
Aneurysms are asymptomatic conditions that can lead to severe and life-threatening problems. Thankfully, there is treatment available and our expert vascular surgeons know how to identify your risks and symptoms. To learn more about this condition and how it can be treated, watch the following video from Dr. Adam A. Richter, MD, FACS, RPVI.
Surgery for Abdominal Aortic Aneurysm
During surgery for abdominal aortic aneurysm (AAA), the weakened aortic wall is replaced with a hollow man made tube (graft).
Reaching the aneurysm
The aorta can be reached through open surgery . Or a less invasive endovascular procedure may be done. Your surgeon will choose the best approach for you.
Open surgery
An incision is made in your abdomen. Once inside, your surgeon gently moves aside your organs to reach the damaged section of the aorta.
Endovascular procedure
Near your groin, the surgeon makes
Placing the graft
The goal is to safely route blood past the aneurysm.
During open surgery
Here is what to expect:
-
The aneurysm is opened and cleaned of any blood clots.
-
The graft is sewn to the aorta.
-
The wall of the aorta is wrapped around the graft to protect it. The wall is then sewn up.
-
The incision site is closed with stitches or staples.
| During open surgery, a graft replaces the weakened section of aortic wall. The wall is wrapped around the graft. |
During an endovascular procedure
Here is what to expect:
-
Watching the catheter on a video monitor, the surgeon places a catheter in the best position. This position is confirmed by a dye study (angiogram).
-
The surgeon guides the graft through the catheter and expands it so blood can flow through it.
-
The blood is now re-routed through the graft and does not fill the aneurysm anymore.
-
The graft is attached inside the artery. It’s held in place with metal springs (stents), hooks, or pins.
-
The catheter is removed. The incision sites are closed with stitches or staples.
| During an endovascular procedure, a graft is inserted inside the aortic wall. The graft is then secured to the aorta above and below the aneurysm. |
Risks and possible complications
Here are potential problems to be aware of:
-
Infection
-
Blood clots in legs
-
Bleeding
-
Kidney failure
-
Respiratory failure
-
Injury to the colon’s blood supply
-
Erectile dysfunction
-
Spinal cord injury
-
Heart attack, stroke, or death
After AAA Surgery
After Open Abdominal Aortic Aneurysm Surgery
You have had surgery to repair an abdominal aortic aneurysm (AAA). This happens when the main blood vessel in your abdominal area weakens and expands like a balloon. Your healthcare provider placed a graft to replace the part of your aorta that was weak. Here’s what you need to know following surgery.
Home care
Recommendations for taking care of yourself at home include the following:
- Don’t do strenuous activity for 4 to 6 weeks after your surgery.
- Ask your healthcare provider how long it will be before you can return to work.
- Gradually increase your activity. It may take some time for you to return to your normal activity level.
- Don’t drive for 2 weeks after surgery or while you are taking opioid pain medicine. Ask someone to take you to any appointments.
- Check your incision every day for signs of infection. These include swelling, redness, drainage, and warmth.
- Keep your incision clean. Wash it gently with soap and water when you shower.
- Don’t lift anything heavier than 5 pounds for 2 weeks after surgery.
- Don’t sit or stand for long periods without moving your legs and feet.
- Keep your feet up when you sit in a chair.
- Take your medicines exactly as directed.
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
- Redness, pain, swelling, or drainage from your incision
- Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
- Sudden coldness, pain, or paleness in your leg
- Loss of feeling in your legs
- Severe or sudden pain in your stomach
- Fail to pass gas
- Bloody bowel movements
- Prolonged constipation
- Nausea or vomiting
- Trouble breathing
- Pain or heaviness in your chest or arms
Still have questions?
Reach out to us to set up an appointment. The Surgical Clinic has locations all throughout Tennessee, including areas such as Nashville, Lebanon, Columbia, and much more. We can address all of your vascular surgery needs, and answer any questions you might have regarding procedures.
After Bypass Surgery
Recovery After Bypass Surgery
If you’ve undergone bypass surgery to help restore blood flow around a blocked artery, there are a few key steps to support your recovery:
- Expect to stay in the hospital for several days, sometimes up to a week, following your procedure.
- Walking is encouraged early on—typically within the first 24 hours after surgery—to help promote healing and circulation. Start slowly and gradually increase both the length and speed of your walks as you gain strength.
- Most people find that full recovery takes between 4 to 8 weeks. During this time, limit strenuous activity and follow your healthcare provider’s guidelines regarding lifting, exercise, and returning to work.
- Pay close attention to how your body feels, and don’t hesitate to ask your medical team questions if you’re unsure about your progress.
By taking recovery one step at a time and attending all follow-up appointments, you’ll give yourself the best chance for a strong and steady return to your usual activities.
VASCULAR PROCEDURE CENTER
VASCULAR SERVICES
Vascular Procedure Centers (VPC)
Our state-of-the-art vascular procedure centers are accredited by the Intersocietal Accreditation Commission and each of the RVT’s are registered through the American Registry of Diagnostic Medical Sonographers (ARDMS). These locations allow you to access advanced laboratory professionals all throughout Tennessee, without the congestion of a hospital setting. While appointments are required, it is often possible to make a ‘same-day’ appointment. Your test results will be sent to your vascular surgeon to help determine a recommended course of treatment.
VPC Columbia | Mt. Juliet | Nashville
Vascular Surgeons
Find a vascular surgeon in Nashville or Middle Tennessee
The Surgical Clinic has board certified vascular surgeons who focus on treating all vascular and endovascular issues including pulmonary embolism, spider veins and varicose veins. Our network of board certified vascular surgeons and vein specialists are able to help patients with everything from common vein problems to serious conditions such as carotid artery disease. To find a provider near you, simply visit our “locations” tab, and choose the closest clinic in your area. We have over 40 surgeons throughout middle Tennessee, offering a variety of vascular surgery options.
Vascular Testing & Diagnostics
PHYSIOLOGIC (NON-IMAGING) TESTING
Physiologic arterial testing is the evaluation of the amount of blood flow to the arms or legs. If narrowing in an artery reduces the amount of blood flow to the arms or legs, we can detect this with physiologic testing. First we listen to the arterial flow and record waveforms of the flow pattern. We take blood pressures at different levels on the arms or legs, and we may have you walk on a treadmill for approximately five minutes to see if blood flow to the legs is reduced further with walking. All of this data helps your physician determine the overall significance of any narrowing and how much blood flow is getting to the legs or arms.
ANKLE/BRACHIAL INDEX
This is a simple physiologic test that involves taking a blood pressure from your arms and your ankles. We obtain a ratio of the ankle pressure to the arm pressure that tells us if the blood flow to your ankles is normal or abnormal. This test is the first step in evaluating the blood flow to your legs and is used to determine which further testing is performed. Arterial Doppler with Segmental Pressures Upper and Lower Extremities: This test involves taking blood pressures from different levels of your legs or arms. We also record waveforms of the blood flow to determine the quality of the blood flow. The blood pressures and waveforms help determine where any arterial narrowing is located.
ARTERIAL DOPPLER WITH TREADMILL
This test may assess your blood pressures in your arms and ankles after you have walked for 5 minutes on a Treadmill. This measures how exercise affects the blood flow to your legs. It is usually conducted after the Ankle/Brachial Index and Segmental Pressure testing is completed.
VASCULAR HEALTH SCREENING
The key to excellent vascular care is proper diagnosis and treatment options. The Surgical Clinic’s ICAVL accredited vascular laboratory offers vascular screening services to assure that you receive proper diagnosis and treatment of your vascular condition. The state-of-the-art vascular ultrasound screening services are painless, fast and accurate. A vascular screening will help identify unnoticed vascular conditions; however, these screening do not take the place of a physical exam.
RAYNAUD’S TESTING
The key to excellent vascular care is proper diagnosis and treatment options. The Surgical Clinic’s ICAVL accredited vascular laboratory offers vascular screening services to assure that you receive proper diagnosis and treatment of your vascular condition. The state-of-the-art vascular ultrasound screening services are painless, fast and accurate. A vascular screening will help identify unnoticed vascular conditions; however, these screening do not take the place of a physical exam.
Vascular Ultrasounds
Vascular ultrasound and physiologic vascular procedures are booked for The Surgical Clinic patients in the Vascular Laboratory in Tennessee. This convenient and comfortable settings allow Registered Vascular Technologists (RVTs) to evaluate the blood supply to and from various parts of the body. This information is obtained without any invasive procedures. After an appointment, you will be able to return to your regular activities. It is important to point out that your care will be delivered by a professional with an RVT certification. The RVT certification, not required in many labs, is the standard at The Surgical Clinics’ labs and helps to assure you that your tests are being conducted by people specialized in these diagnostic procedures. We have a variety of locations across Tennessee, so whether you live in Nashville or Dickson TN, we’ve got a provider for you.
PAD Screening
Learn more about how and why you should get screened for peripheral arterial disease.
Common Vascular Surgeries
Carotid Endarterectomy:
Stroke Prevention:
Carotid endarterectomy is a surgical procedure aimed at preventing strokes by removing plaque buildup in the carotid arteries, which are the major blood vessels in the neck leading to the brain.
Risk Reduction:
This procedure is particularly beneficial for patients with significant carotid artery narrowing (stenosis), as it reduces the risk of a stroke caused by the dislodgment of plaque fragments.
Quick Recovery:
Carotid endarterectomy is a well-established procedure with a relatively quick recovery time. Many patients can return to normal daily activities within a few weeks. In addition to improving blood flow to the brain, the procedure significantly reduces stroke risk.
Endovascular Aneurysm Repair (EVAR):
Minimally Invasive:
EVAR is a minimally invasive procedure used to treat abdominal aortic aneurysms (AAAs). During the procedure, a stent-graft is inserted through a small incision, usually in the groin, and guided into place inside the aorta. This reinforces the weakened artery wall and reduces the risk of rupture.
Lower Risk:
Compared to traditional open surgery, EVAR is associated with lower morbidity and mortality rates. It often results in shorter hospital stays and a quicker return to normal activities.
Regular Surveillance:
Patients who undergo EVAR require regular follow-up appointments and imaging to monitor the stent-graft’s position and ensure its continued effectiveness in preventing aneurysm expansion.
Peripheral Artery Bypass Surgery:
Blood Flow Restoration:
Peripheral artery bypass surgery is performed to restore proper blood flow in the legs or arms by creating a bypass around blocked or narrowed arteries. It can alleviate pain and improve mobility.
Autologous Grafts:
Vascular surgeons commonly use autologous grafts, which are segments of the patient’s own veins, to create the bypass. This reduces the risk of graft rejection.
Lifestyle Improvement:
For individuals suffering from severe peripheral artery disease (PAD), bypass surgery can significantly enhance their quality of life, allowing them to walk longer distances and engage in physical activities without pain.
These procedures, performed by vascular surgeons, play a crucial role in treating vascular conditions and improving patients’ overall health and well-being. Each procedure has its unique benefits and considerations, and the choice of treatment depends on the patient’s specific condition and medical history.
Why Choose Vascular Surgery at TSC in Nashville?
Highly Respected
The Surgical Clinic is one of Middle Tennessee’s most respected surgical practices. Patients across the Southeast and throughout the country trust us for our high standards, compassionate care, and innovative medical solutions.
Vascular Specialists
We recruit Greater Nashville’s most skilled surgeons. Our vascular surgeons hold certifications from the Vascular Surgery Board of the American Board of Surgery. They prioritize minimally invasive procedures to achieve the best results possible, even after recovery.
Teamwork
At The Surgical Clinic, our vascular surgeons collaborate to provide our patients with individualized care. Our dedicated team members also collaborate with experts in various medical disciplines to guarantee we address your unique needs.
Patient-First Approach
Our goal is to have you feel confident going into surgery so you can focus your energy on improving. In addition to individualized care, we offer an online library to educate our patients about vascular surgery procedures, what to expect with surgery, and more.
Vascular Surgery FAQ
1. When is vascular surgery necessary?
Vascular surgery may be necessary to treat conditions such as blocked arteries (atherosclerosis), aneurysms, varicose veins, blood clots, and other vascular diseases.
2. What are the common vascular conditions treated by vascular surgeons?
Common conditions treated include peripheral artery disease (PAD), deep vein thrombosis (DVT), carotid artery disease, aortic aneurysms, and varicose veins.
3. What are the different types of vascular procedures?
Vascular procedures include angioplasty and stenting, bypass surgery, endarterectomy, thrombectomy, and aneurysm repair, among others.
4. How do I prepare for vascular surgery?
Preparation may involve fasting before surgery, discontinuing certain medications, and discussing any underlying medical conditions with your surgeon.
5. What should I expect during vascular surgery?
During surgery, you will typically be under anesthesia, and the surgeon will make incisions as needed to access and repair the affected blood vessels.
6. Is vascular surgery painful?
Pain management is an important aspect of vascular surgery. Your medical team will provide pain relief options to ensure your comfort during recovery.
7. How long does vascular surgery recovery take?
Recovery times vary depending on the procedure and individual factors. Some procedures may require a short recovery period, while others may take weeks or months.
For example, minimally invasive treatments like sclerotherapy or endovascular vein therapy (used for varicose and spider veins) are typically office-based and offer a quicker recovery—most patients can return to work the next day, with most healing occurring within 1–2 weeks. Bruising and swelling are common, but wearing compression stockings during this time can help. It’s important to start walking soon after the procedure, gradually returning to normal activities, though strenuous exercise (like running or jumping) should be avoided for two weeks.
More involved procedures, such as vein stripping (removal of the saphenous vein), are performed in a hospital setting. Recovery for these surgeries generally takes 2–4 weeks. Bruising and swelling are common for the first couple of weeks, and compression stockings are again encouraged. Patients are usually advised to start walking promptly, slowly increasing activity levels and avoiding strenuous tasks during early recovery. Many people can return to work within 1–2 weeks.
Procedures like balloon angioplasty and stenting, which open narrowed arteries and insert a stent to improve blood flow, may require a hospital stay of several days. Bruising may occur in the first few days, but walking is encouraged early on with gradual increases in activity. Avoid sitting or standing for long periods, and elevate your legs when lying down. Full healing for angioplasty and stenting can take up to 8 weeks.
For bypass surgery, where blood flow is routed around a blocked artery, recovery can take 4–8 weeks. Walking is usually started within 24 hours post-surgery, with slow and steady increases in duration and intensity as healing progresses.
Your surgeon and care team will provide detailed, personalized instructions to support your recovery and help you return to your normal activities as safely and quickly as possible.
8. What are the potential risks and complications of vascular surgery?
Risks may include infection, bleeding, blood clots, and reactions to anesthesia. Your surgeon will discuss these risks with you before the procedure.
9. Will I have scars after vascular surgery?
Most surgical procedures leave some degree of scarring. The size and visibility of the scar will depend on the type of surgery and your body’s healing process.
10. Can vascular surgery prevent future vascular problems?
Vascular surgery can address existing issues and improve blood flow. Lifestyle changes and ongoing medical management may be necessary to prevent future problems.
Vascular Surgery Blogs
Carotid Artery Disease: A Silent Stroke Risk You Need to Know About
February is Heart Health Month, making it a...
Common Vein Conditions and Effective Treatments
Sometimes, leg pain and swelling are caused by...
Aortic Aneurysms: When to Monitor and When Surgery is Necessary
Heart disease is the leading cause of death in...



