Deep Vein Thrombosis (DVT)
What Is Deep Vein Thrombosis?
Several types of blood clots can occur in the body, and some are more serious than others.
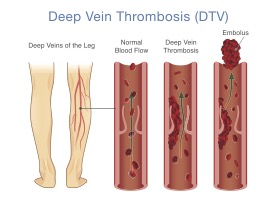
Deep Vein Thrombosis (DVT) is a common type of blood clot that affects millions of people worldwide every year. It forms in the deep veins of your body, usually in the legs.
Fortunately, several treatment options can help manage DVT and prevent future clots from forming. But if not treated promptly, DVT can lead to serious health complications such as pulmonary embolism (PE.)
In this blog, we’ll explore DVT, its risk factors and symptoms, and the latest treatment options available to help those affected by this condition.
UNDERSTANDING DVT
DVT is a blood clot that forms in a large vein deep inside a leg, arm or another part of the body. The clot can partially or completely block blood flow through the vein.
DVT is different from blood clots in arteries. A blood clot in an artery, usually in the heart or brain, is called arterial thrombosis and is the type of blood clot that can cause a heart attack or stroke. In the case of DVT, the most concerning complication is a pulmonary embolism (PE), which occurs when a blood clot breaks off from a deep vein, travels through the bloodstream, and blocks a blood vessel in the lungs. Just like a heart attack or stroke, PE can be very dangerous and life-threatening.
You might hear your healthcare provider use the term venous thromboembolism (VTE) to describe both DVT and PE. They use the term VTE because the two conditions are closely related, and their prevention and treatment are similar.
Sometimes, those with DVT will notice swelling, pain, and discomfort. However, more times than not, DVT has very few symptoms and sometimes goes unnoticed until it causes serious complications, such as PE.
DVT RISK FACTORS AND SYMPTOMS
One of DVT’s most common risk factors is immobility, which can slow blood flow and increase the risk of blood clots. This can happen if you’re on a long flight or car ride, bedridden due to illness, or sitting or lying down for long periods.
Other factors that can increase the risk of DVT include:
- Smoking
- Genetic predisposition
- Injuries to the veins (from surgery or trauma)
- Certain medical conditions (such as cancer or heart failure)
- Hormonal changes (such as during pregnancy or while taking hormonal contraceptives)
It can be hard to detect DVT, and usually, no immediate symptoms exist. However, if you have been immobile or have any of the above risk factors and are noticing one or more of the following symptoms, it might indicate DVT.
- Swelling in the affected area
- Warmth in the affected area
- Acute shortness of breath or rapid shallow breathing
- Fast pulse
- Coughing up blood
- Chest pain or discomfort
- Lightheadedness, dizziness, or fainting
- Pain in the affected area (cramping or soreness)
- Redness or discoloration of the skin over the affected area
- Enlarged veins that are visible just below the skin’s surface
- Tenderness when the affected area is touched or squeezed
It’s important to note that some people with DVT may not experience any symptoms, especially in the early stages of the condition. If you have concerns about DVT or are experiencing any of the symptoms above, it’s important to seek medical attention promptly.
HOW TO AVOID GETTING DVT
DVT can be a serious and potentially life-threatening condition, but there are several steps you can take to help reduce your risk of developing this type of blood clot.
Here are some tips to help you avoid getting DVT:
- Get moving: If you sit for long periods of time, take breaks and move around every hour or so to improve blood flow. This is especially important for long flights or road trips. If you are traveling, take breaks to move around and stretch your legs.
- Wear compression stockings: Compression stockings can help improve blood flow and reduce the risk of developing blood clots. These stockings could be especially useful during times when you will be sitting for an extended time.
- Maintain a healthy weight: Being overweight or obese can increase the risk of developing DVT. Adopt a healthy lifestyle that includes exercise and a healthy diet.
- Quit smoking: Smoking can damage your blood vessels and increase the risk of developing DVT. If you are a smoker, you should stop immediately.
- Stay hydrated: Drinking plenty of water can help prevent dehydration, which can make blood more likely to clot.
- Manage other health conditions: It is important to manage conditions such as high blood pressure and diabetes, as these conditions can increase the risk of DVT.
For most people, adopting a healthy lifestyle and following these tips can help reduce the risk of developing DVT. However, if you already have a blood clot or are at high risk for DVT, your doctor may recommend additional measures.
TREATING DVT
Most often, a blood clot is treated with medicines that help to either thin the blood or dissolve the clot. These medications can vary from blood thinners (anticoagulants) to thrombolytics, which are powerful medications that can dissolve blood clots quickly.
Medications also help prevent pulmonary embolism and other complications, but this is not true for everyone. Depending on your health and the size and location of the blood clot, your healthcare provider may recommend one or more of the following options to treat venous thrombosis:
- Catheter delivering medication
- Balloon angioplasty
- Embolus filter
Here are three of the most common procedures used for the abovementioned treatment options:
- Thrombolysis: Also known as thrombolytic therapy, this procedure is used to dissolve a large blood clot and is typically reserved for severe cases of DVT or for cases in which other treatment options have not been successful.
A catheter (thin tube) is inserted into the vein during the treatment. X-rays are taken of the vein and the clot. Then, clot-dissolving medicine is delivered directly to the clot through the catheter. The medication works by breaking down the proteins that hold the clot together, allowing it to dissolve and restoring blood flow to the affected area. In some cases, a mechanical device is also used to break up the clot. Thrombolysis is generally considered a more aggressive and invasive treatment option for DVT. As such, it is typically only used in certain circumstances, such as when a person is at high risk for pulmonary embolism or when other treatments have not been successful.
In some people, thrombolysis is a very effective treatment for blood clots. However, it does carry the risk of bleeding complications. The risks and benefits of the treatment should be carefully weighed in each individual case.
- Angioplasty: This treatment option for DVT involves using a balloon-tipped catheter to widen the narrowed or blocked vein to restore blood flow to the affected area. It is often used in cases where blood thinners or other conservative treatments are ineffective, or a person is at high risk of severe complications such as pulmonary embolism.
While under local anesthesia, your surgeon will insert a catheter into the affected vein. X-rays are used to position the catheter. Once the catheter is in place, the balloon is inflated to compress the clot and widen your vein. In some cases, a wire mesh device, called a stent, may also be placed in your vein to help keep it open.
Like any medical procedure, angioplasty for DVT carries some risks, such as bleeding, infection, and damage to the vein. In addition, it may not be suitable for all individuals with DVT, depending on the location and severity of the clot.
- Inferior Vena Cava Filter: The purpose of an Inferior Vena Cava (IVC) filter is to trap blood clots that may break free and travel through the bloodstream to the lungs. It is usually recommended for patients at high risk of developing PE but who cannot take blood-thinning anticoagulant medications. The filter may also be used in patients who have already developed PE despite receiving anticoagulant therapy.
The filter is a small, cage-like device inserted via a catheter into the inferior vena cava, the large vein that carries deoxygenated blood from the lower body back to the heart. It works by physically blocking these blood clots from reaching the lungs, thereby reducing the risk of PE.
Complications associated with IVC filters may include filter migration, filter fracture, or the formation of blood clots around the device. Therefore, the decision to use an IVC filter should be made on a case-by-case basis, carefully considering the potential benefits and risks for each patient. Your healthcare provider will discuss the risks and benefits of this procedure if it’s recommended for you.
Each case of DVT requires individualized treatment. Your healthcare provider can give you more information about treating your blood clot, including information about these and other DVT treatments available.
HOW TO KEEP YOUR VASCULAR HEALTH AFTER HAVING DVT TREATMENT
After receiving treatment for DVT, there are several steps you can take to help maintain your vascular health and reduce your risk of developing another blood clot in the future.
Here are some tips:
- Follow your doctor’s instructions: It is important to follow your doctor’s instructions regarding medication, diet, exercise, and lifestyle changes after treatment for DVT.
- Take prescribed anticoagulant medications: Anticoagulant medications, such as heparin or warfarin, are often prescribed after DVT treatment to prevent further blood clots from forming. It is important to take these medications as prescribed and to keep all follow-up appointments with your doctor.
- Stay active: Your doctor may recommend certain exercises or activities that are safe for you. These exercises are important as regular physical activity can help improve blood flow and reduce the risk of blood clots.
- Maintain a healthy weight: Being overweight is known to increase the risk of developing DVT. Eating a healthy diet and staying physically active can help you maintain a healthy weight.
- Stop smoking: If you smoke, talk to your doctor about ways to quit. Smoking can damage your blood vessels and increase the risk of developing DVT.
- Wear compression stockings: Your doctor may recommend wearing compression stockings after DVT treatment. Compression stockings can help improve blood flow and reduce the risk of developing blood clots.
- Manage other health conditions: Certain medical conditions, such as high blood pressure or diabetes, can increase the risk of developing DVT. Managing these conditions through medication, lifestyle changes, and regular medical care is essential.
By following these steps, you can help maintain your vascular health and reduce the risk of developing another blood clot after DVT treatment.
SCHEDULE AN APPOINTMENT WITH A VASCULAR SURGEON IN NASHVILLE, TN
Whether you believe you have DVT or another vascular disease, many of our experienced and compassionate vascular surgeons here at The Surgical Clinic in Middle Tennessee are accepting new patients.
Contact us to book your appointment or if you would like to learn more about DVT treatment options. We’d be happy to answer any questions that you have.
Deep Vein Thrombosis (DVT) is a serious condition that occurs when a blood clot forms in a deep vein, typically in the legs or pelvis. Recognizing the symptoms of DVT is crucial for early detection and prompt treatment. Here’s what you need to know:
Symptoms of DVT may include:
- Swelling in the affected leg, ankle, or foot.
- Pain or tenderness, often described as a cramping or soreness, in the affected leg.
- Warmth and redness over the affected area.
- Skin that feels tight and shiny.
- Unexplained pain or discomfort, especially when standing or walking.
If you experience any of these symptoms, especially if they are sudden or severe, it’s essential to seek medical attention promptly. DVT can lead to serious complications, such as a pulmonary embolism (when the clot travels to the lungs), so early diagnosis and treatment are crucial for your overall health.
Remember, if you’re at higher risk for DVT due to factors like prolonged immobility, recent surgery, or a history of clotting disorders, it’s even more important to be vigilant about recognizing these symptoms.
When to See a Vascular Surgeon for DVT
If you suspect you have Deep Vein Thrombosis (DVT), consulting a vascular surgeon is a wise step toward proper diagnosis and treatment. Vascular surgeons specialize in managing conditions affecting the veins and arteries. Here’s when you should consider seeing a vascular surgeon for DVT:
-
Persistent Symptoms: If you experience persistent leg swelling, pain, or discomfort that doesn’t improve with rest or over-the-counter treatments, it’s time to consult a vascular surgeon.
-
Risk Factors: If you have known risk factors for DVT, such as a history of blood clots, recent surgery, pregnancy, or prolonged immobility, it’s wise to consult a specialist even if you’re not currently experiencing symptoms.
-
Symptoms of Pulmonary Embolism: Symptoms like sudden shortness of breath, chest pain, rapid heartbeat, or coughing up blood can indicate that a blood clot from DVT has traveled to your lungs. In this case, seek emergency medical attention, and follow up with a vascular surgeon for further evaluation.
-
Preventive Measures: If you’re planning surgery, a long flight, or any situation that could increase your risk of DVT, consulting a vascular surgeon for preventive measures and advice on reducing your risk is a smart move.
Remember, early intervention can prevent complications and ensure the best possible outcomes. Your vascular surgeon will guide you through appropriate tests, treatments, and lifestyle adjustments tailored to your individual needs.
Preventing Deep Vein Thrombosis (DVT)
Preventing Deep Vein Thrombosis (DVT) is essential to maintain vascular health. Here are some steps you can take to help reduce your risk:
-
Stay Active: Regular physical activity helps improve blood circulation. If you have a sedentary job or lifestyle, take breaks to walk around, stretch your legs, and keep blood flowing.
-
Maintain a Healthy Weight: Excess weight can strain your circulatory system. Aim for a balanced diet and exercise routine to maintain a healthy weight.
-
Stay Hydrated: Proper hydration supports blood flow and prevents blood from becoming too thick. Drink water throughout the day.
-
Avoid Prolonged Immobility: If you’re on a long flight or road trip, take breaks to walk and stretch. When sitting for extended periods, flex your ankles, rotate your feet, and perform calf raises.
-
Quit Smoking: Smoking damages blood vessels and increases the risk of clot formation. If you smoke, seek help to quit.
-
Follow Medical Advice: If you have known risk factors for DVT, such as a family history of clotting disorders, discuss preventive measures with your healthcare provider.
-
Compression Stockings: If recommended by your doctor, wear compression stockings to help improve blood circulation and reduce the risk of blood pooling in your legs.
-
Medications: If you’re at high risk of DVT due to surgery or medical conditions, your doctor might prescribe blood-thinning medications. Follow their instructions carefully.
Remember, prevention is key to avoiding DVT and its potential complications. By adopting these healthy habits and seeking medical guidance when needed, you can significantly reduce your risk of developing this condition.
VASCULAR SURGEONS AT THE SURGICAL CLINIC

Dr. Thomas Beazley
Vascular Surgeon
VIEW PROFILE

Dr. Julia Boll
Vascular Surgeon
VIEW PROFILE

Dr. JimBob Faulk
Vascular Surgeon
VIEW PROFILE

Dr. Brian Kendrick
Vascular Surgeon
VIEW PROFILE

Dr. Billy J. Kim
Vascular Surgeon
VIEW PROFILE

Dr. Allen Lee
Vascular Surgeon
VIEW PROFILE

Dr. Caroline Nally
Vascular Surgeon
VIEW PROFILE

Dr. Elizabeth F. Nelson
Vascular Surgeon
VIEW PROFILE

Dr. Adam Richter
Vascular Surgeon
VIEW PROFILE

Dr. Mark Shelton
Vascular Surgeon
VIEW PROFILE

Dr. Todd H. Wilkens
Vascular Surgery
VIEW PROFILE

Dr. Patrick Yu
Vascular Surgeon
VIEW PROFILE
VASCULAR SURGERY ARTICLES
Common Vein Conditions and Effective Treatments
Sometimes, leg pain and swelling are caused by...
Aortic Aneurysms: When to Monitor and When Surgery is Necessary
Heart disease is the leading cause of death in...
Vein Pain: Solutions for Varicose Veins
Many people don’t associate veins with pain, but...
Top Docs at The Surgical Clinic
Celebrating The Surgical Clinic’s Top Docs...
Stroke Prevention: A Comprehensive Guide | B.F.A.S.T.
Strokes can be devastating, often leaving...
Vascular Surgery: How Vascular Conditions Are Diagnosed And Treated
Seeking clarity on vascular surgery how vascular...






