Millions of Americans suffer from varicose veins. Varicose veins are unsightly, painful, and can disrupt your body’s ability to circulate blood effectively. If you have a diagnosis of varicose veins, you may have questions.
Here are a few answers to frequently asked questions you may have about varicose veins.
What Are Varicose Veins?
Varicose veins are easily visible through the skin and are either flat or raised and bulging. On the other hand, spider veins are a type of diseased veins and get their name for their web-like appearance. In contrast, varicose veins are flesh-colored, purple, blue, or red. These veins are predominantly found on the back legs or calves, although they can occur anywhere on the body.
What Causes Symptomatic Varicose Veins?
Varicose veins occur when valves that push blood through the veins to the heart are damaged or malfunction. Blood that does not travel to the heart pools and causes discoloration or the veins to bulge. As a result, there are several risk factors associated with varicose veins, including:
- Age. Natural valve degeneration occurs as a person ages. The weakened valves cannot push the blood toward the heart.
- Pregnancy. Blood volume increases and blood circulation to the legs and pelvis decreases during pregnancy. Changes in volume and circulation support the developing baby.
- Obesity. Excess weight places pressure on veins, causing them to work harder to circulate blood.
- Sitting or standing for long periods. Remaining in the same position for several hours restricts blood flow.
- Family history. Certain genetic diseases and conditions affect vein functionality.
Changes in a woman’s hormone levels place women at a higher risk of developing varicose veins. These types of changes typically occur after menopause or when women take birth control.
What Are the Symptoms of Varicose Veins?
Patients with varicose veins often experience no symptoms, aside from the discoloration and bulging veins. However, others will suffer a variety of symptoms, including:
- Itching and burning
- Muscle cramps near the affected veins
- Discomfort
Prolonged periods of sitting or standing will sometimes worsen varicose vein pain.
Are All Varicose Veins the Same?
No, your body has deep, superficial, and perforator venous systems. Any of these systems can develop varicose veins and have a range of severity. Every patient has different anatomy, risk factors, and condition, so no varicose vein is identical to the next.
How Common are Varicose Veins?
Varicose veins are common; they affect about 1 in 3 adults. However, certain risk factors can increase the chances of someone developing varicose or spider veins. People often develop varicose and spider veins in their legs and feet.
Are Varicose Veins a Serious Health Concern?
The condition generally worsens over time and, left untreated, can cause symptoms. Extreme cases can lead to venous insufficiency, preventing blood from flowing back toward the heart.
Do Only Older Women have Varicose Veins?
No, any person at any age can develop varicose veins. Men and women in their 20s to 90s have had varicose veins. However, certain risk factors increase the chances of having them, like age, gender, lifestyle, and family history.
How do You Prevent Varicose Veins?
There is no cure-all to prevent varicose veins, but there are measures you can take to decrease the severity of symptoms. Eating healthy, exercising regularly, avoiding standing or sitting for long periods, maintaining healthy body weight, wearing compression stockings, and elevating your legs all help minimize varicose vein symptoms.
What Are the Complications Associated With Varicose Veins?
Decreased blood flow can cause several potentially serious complications, including:
- Bleeding. Affected veins are thin and damaged, so if the patient bumps or injures their leg, excessive bleeding can occur.
- Blood clots. Superficial thrombophlebitis, or clots that form just beneath the skin, is characterized by pain and swelling.
- Ulcers. Decreased blood flow causes blood to pool and a painful sore to form.
- Varicose eczema. Red, flaky, irritated skin can crust over and blisters form at the affected area.
- Chronic venous insufficiency. Decreased blood flow disrupts the skin and blood’s ability to exchange waste, oxygen, and nutrients.
Deep vein thrombosis, or DVT, is a serious condition that occurs when a blood clot forms in the leg. In fact, DVT is very painful. Furthermore, without immediate treatment, a blood clot can travel to the lungs. A blood clot in the lungs is a life-threatening condition known as pulmonary embolism.
How Will My Doctor Diagnose Vein Disease?
Your doctor will perform a physical examination and ask about any pain, swelling, or other symptoms you’re experiencing. Next, they will order an ultrasound test if they suspect you have a blood clot. Alternatively, your doctor may suspect you have other complications and order an ultrasound as a result.
Why do I Need an Ultrasound of My Legs?
Symptoms may or may not be visible. An ultrasound allows a doctor to examine the major veins inside the leg to check for venous insufficiency or varicose veins under the skin. The non-invasive exam allows the healthcare provider to detect the source of the vein issue, which is critical to proper treatment.
How Are Varicose Veins Treated?
 Superficial varicose veins are unsightly but typically do not require any medical treatment. In this case, your doctor will recommend you do the following to alleviate symptoms:
Superficial varicose veins are unsightly but typically do not require any medical treatment. In this case, your doctor will recommend you do the following to alleviate symptoms:
- Exercise
- Lose weight
- Elevate your legs
- Avoid sitting or standing for long periods of time
- Wear compression socks to help veins push blood from the legs to the heart
- Take over-the-counter anti-inflammatory medications, including aspirin or ibuprofen
Additionally, at-home treatments alleviate the pain and swelling of varicose veins and prevent the condition from getting worse. Further helpful therapies to treat or eliminate varicose veins include:
- Sclerotherapy. During this procedure, a chemical or foam is injected into the vein, collapsing its walls. However, this outpatient procedure requires no anesthesia.
- Laser surgery. This non-invasive procedure uses lasers to send powerful beams of light into the affected veins. Usually, this is an outpatient procedure.
- Ablation. Your doctor inserts a small catheter into the affected veins and uses either lasers or a radio-frequency device to superheat and collapse the veins. Usually, this provides excellent results.
- Vein stripping. Affected veins are tied off at the point before they meet a larger vein. The doctor removes the veins piece by piece through a series of small incisions.
Advanced cases, or those that were not cured by the above-mentioned procedures, often require endoscopic vein surgery. During this procedure, the doctor inserts a small camera into the leg and uses a scalpel to remove the affected vein.
How does Laser Treatment Work?
Heat from the laser in the form of light closes and shrinks the varicose vein. The laser causes scar tissue to form within the blood vessel, which seals off the vein. Blood then finds nearby veins to flow through.
What is a Phlebectomy of Varicose Veins?
A microphlebectomy or ambulatory phlebectomy is when a healthcare provider makes tiny incisions and removes the veins. The procedure uses only local anesthetic and requires no stitches. A phlebectomy is an in-office procedure that only takes about an hour.
Is It Bad to Lose a Vein?
Your legs have many veins. When one unhealthy vein is closed, the blood will find another vein that’s healthy to flow through. Losing one vein does not negatively affect your health.
Will Insurance Cover the Treatment Cost?
It is essential to check with your insurance company before making your appointment with a surgeon. The Surgical Clinic accepts most insurance coverage, but you will want to ensure that your specific policy is included. A call to your insurance company will provide you peace of mind that your procedure will be covered.
Can Varicose Veins Return After Treatment?
Modern varicose vein treatments have a very high success rate. However, there is no cure for weak vein valves or venous insufficiency. As a result, more abnormal veins can develop into varicose and spider veins.
Ultrasounds can track the progression of weak valves, and ongoing treatment can keep symptoms under control. Wearing compression socks and stockings as much as possible during the day is the most effective way to slow down new varicose veins.
How do I Put on Compression Stockings?
While compression socks and stockings are highly effective for easing symptoms and preventing new varicose veins, many people wear them incorrectly. Wearing compression stockings with folds or bunching puts you at risk of circulation loss and can lead to complications. Here’s how to put on compression stockings the right way:
- Palm up down the back of the stocking down to the heel pocket. Tuck the thumb into the heel pocket and hold it like a puppet. Turn the sock inside out and stop at the heel point. Remove your hand and flip over the stocking; you will see a “toe tunnel.”
- Find the bottom of the stocking, by locating the heel pocket, and face it towards the ground. Put all fingers inside the “toe tunnel,” stretch it as wide as possible, and pull the sock halfway up the foot. Grab the end of the hose and pull it over the ankle and bottom of the leg.
- Grab a pair of sturdy rubber gloves with texture. Grab the stocking just above the heel and tug towards the ankle. Then grab the rest of the stocking and flatten it out. Repeat the “tugging and flattening” until the stocking reaches the top of your shin.
- Take off the rubber gloves and grab the top band. Pull it towards the knee, but not all the way up. The band should not touch the back bend of the leg. Make sure the stocking is at least two fingers below the knee.
- Slide hands down the leg to check for wrinkles. If there are wrinkles, reapply gloves and smooth the crease out with a gentle upward motion.
How Long does It take to Complete the Treatment?
After an ultrasound, your doctor will likely schedule you for treatment in one to two weeks. Depending on the type of treatment, you will probably finish the procedure in an hour. You can immediately go back to regular daily activities. There is no recovery time for a majority of vein treatments.
Is It Safe to get Vein Treatment While I am Pregnant?
Varicose veins are common in pregnant women. However, if pregnant, you should not have elective vein treatments until after you finish breastfeeding. Remember that varicose veins during pregnancy typically resolve on their own after giving birth without any treatment.
Varicose veins are a common problem that can lead to several dangerous conditions, including deep vein thrombosis.
March is Deep Vein Thrombosis (DVT) Awareness Month
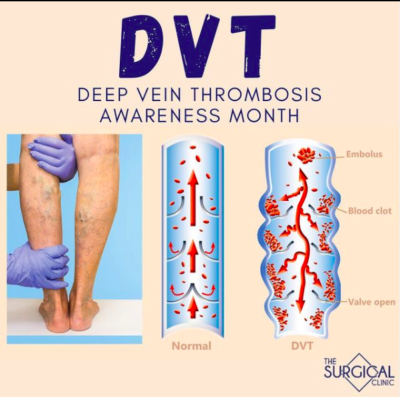 DVT is a blood clot that develops, usually in the deep veins of the legs.
DVT is a blood clot that develops, usually in the deep veins of the legs.
DVT can be very painful, and if not treated immediately, a blood clot can travel to the lungs, a life-threatening condition known as pulmonary embolism.
Lifestyle changes that can help prevent DVT:
– Quit smoking
– Lower your blood pressure
– Lose weight
- Avoid sitting for long periods of time
– Exercise
If you have any more questions or suspect you are suffering from varicose veins, contact the professionals at The Surgical Clinic. We can diagnose your condition and determine the best treatment for you.
Meet Our Vascular Surgeons
Allen P. Lee Jr. MD, FACS, RPVI
Downtown Clinic, The Vein Centre – Mt. Juliet
Todd H. Wilkins, MD
Summit Clinic, The Surgical Clinic – Rutherford
Adam A. Richter, MD, RPVI
Skyline Clinic
Julia (Julie) Boll, MD, RPVI
St. Thomas West, The Vein Centre – Mt. Juliet
Jeffery B. Dattilo, MD, FACS
St. Thomas West
Bryan T. Fisher Sr., MD
Downtown Clinic, The Surgical Clinic – Ashland City
Roger A. Banou, MD, FACS
The Vein Centre – Aspen Grove, Belle Meade, Mt. Juliet

