Cholecystectomy, or surgical gallbladder removal, is a frequently performed procedure that can alleviate discomfort from gallstone pain without a lengthy hospital stay. Generally regarded as safe, this operation typically involves minimal risk of complications.
In addition, minimally invasive laparoscopic (video-assisted) techniques have dramatically reduced surgical and healing timeframes. Remarkably, the majority of individuals can return home on the same day they have the procedure.
If you’re considering laparoscopic gallbladder removal, keep reading to learn what you need to know about recovering from this outpatient surgery.
What is a Gallbladder?
The gallbladder plays a vital role in the digestive system. It is a small, pear-shaped organ below the liver that stores bile; bile, a liquid produced by the liver.
Once you eat, the gallbladder releases bile into the small intestine to help break down fats, making them easier for the body to absorb and use. Essentially, the gallbladder acts as a storage unit that ensures bile is available when needed for digestion.
How does not having a gallbladder affect you?
While the gallbladder aids digestion, living without a gallbladder does not change your quality of life. There are typically no long-term effects to worry about after surgery. Though, you may need to make minor changes to your diet.
WHAT IS GALLBLADDER SURGERY?
The medical term for gallbladder surgery is cholecystectomy (KOL-i-si-STEK-tuh-mee).
A cholecystectomy, primarily performed to address gallstones, provides numerous benefits and promising results for those suffering from gallbladder issues.
One of the primary benefits is pain relief. Gallstones often cause significant discomfort, and conservative treatments, like dietary changes, typically cannot prevent these stones from recurring. In contrast, a cholecystectomy effectively eliminates this problem by removing the gallbladder, thereby preventing the return of gallstones for most patients.
Post-surgery, most individuals experience minimal digestive issues. While the gallbladder plays a role in digestion, it is not essential for healthy digestion overall. Though some people may encounter occasional loose stools after the procedure, this issue generally resolves itself over time.
Benefits of Cholecystectomy
A cholecystectomy offers notable benefits, including:
- relief from the pain associated with gallstones
- a lower risk of gallstone recurrence
- minimal digestive issues
- a relatively quick recovery period, particularly with the laparoscopic method
Always consult with your healthcare team to discuss any post-surgery symptoms or concerns.
WHAT DOES CHOLECYSTECTOMY MEAN?
Broken down, cholecystectomy means:
Chole = bile, Greek
Cysits = bladder, Latin
Ectomy = surgical removal, Greek
There are two primary methods for gallbladder removal: laparoscopic and open cholecystectomy.
GALLBLADDER REMOVAL AND POST-OP SURGICAL STAY
When it comes to gallbladder removal, or cholecystectomy, surgeons can choose between two main surgical techniques: laparoscopic cholecystectomy and open cholecystectomy. The choice of method often depends on the patient’s specific condition and medical history.
Open Cholecystectomy
A traditional open cholecystectomy procedure typically requires two to three days of post-operative hospital stay. This invasive, open procedure requires the surgeon to make a six-inch incision under the right side of the ribcage, moving the surrounding muscle and tissue to remove the gallbladder.
- Recovery: After gallbladder removal, the incision is sutured, and the patient is moved to a recovery area.
- Duration: Similar to the laparoscopic approach, this procedure also typically takes 1 to 2 hours.
Although more invasive, an open cholecystectomy may be necessary in cases where the laparoscopic method is not feasible, ensuring the patient’s safety and providing the surgeon better visibility and access.
After the surgery, your doctor may insert one or more drains into the incision to allow drainage of fluids or pus. They will likely remove the drains after a couple of days.
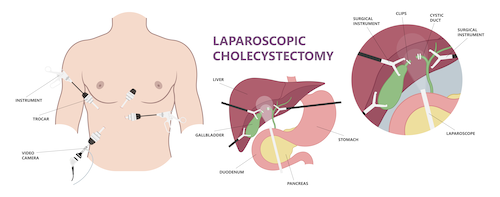
Laparoscopic Cholecystectomy
In comparison, a laparoscopic procedure is much less invasive. The surgeon makes four small incisions in the abdomen instead of one long cut. Then, the surgeon feeds a small video camera through one of the incisions, allowing the surgeon to view the interior of the abdomen on a monitor. Special surgical instruments are then inserted through the other incisions to carefully remove the gallbladder.
- Imaging Tests: If necessary, imaging tests like X-rays or ultrasounds may be conducted to inspect for gallstones or other complications in the bile duct.
- Duration: The procedure typically lasts between 1 to 2 hours.
Laparoscopic cholecystectomy is minimally invasive and generally has a shorter recovery time.
This less invasive approach often equals no hospital stay for most patients—meaning you can recover at home.
However, if the surgeon encounters complications, such as extensive scar tissue from previous surgeries, it may become necessary to switch to an open cholecystectomy.
GALLBLADDER REMOVAL COST
Depending on your health insurance, laparoscopic gallbladder surgery can cost more than open surgery. The best way to determine the cost of the procedure is to consult your surgeon and discuss the best options.
Without insurance, gallbladder removal surgery can cost between $10,000 and $55,000. However, we gladly offer uninsured patients affordable payment options and financial assistance
EXPECTED PAIN
Post-surgical pain is a significant concern for many cholecystectomy patients. Even though every surgical procedure has some pain, the discomfort with gallbladder removal (especially when done laparoscopically) is typically minimal. The doctor may prescribe a pain medication or recommend that you take an over-the-counter pain medicine, such as acetaminophen or ibuprofen.
Some patients also experience shoulder pain following laparoscopic gallbladder removal surgery. This temporary discomfort comes from gas left in your abdomen during surgery.
Along with incision and shoulder pain, you may feel throat discomfort. This pain occurs because general anesthesia used during surgery requires a breathing tube. The placement and removal of the tube may irritate your throat in the day or days following the procedure.
Severe pain and cramping are not normal following laparoscopic cholecystectomy. If you experience these symptoms, call your doctor immediately.
RETURNING TO ACTIVITY AFTER GALLBLADDER REMOVAL
How soon can you resume your everyday activities after surgery? The answer to this question depends on your normal routine, overall health, and body’s reaction to the surgery. Don’t expect to resume a strenuous gym routine or return to a manual labor job immediately after your operation.
Recovery time can vary based on the surgical method used and the patient’s overall health.
Typically, open cholecystectomy takes 4-6 weeks to recover, while laparoscopic surgery takes about 1-2 weeks to recover. After recovery, the patient can resume regular activities, including work.
Even though laparoscopic surgery provides patients with a shorter healing time, you will still need to take it easy for several days after the procedure. Avoid heavy lifting and physical activity for the first week or two following your surgical discharge.
It’s possible, in some cases, to return to work or school during the first few weeks of your recovery period—especially if you sit at a desk or have a sedentary job. Your doctor will advise you when you can return to other activities, such as exercising or engaging in physically demanding tasks.
Again, this depends on your physical state and how your body reacts to the procedure. The doctor may want you to rest until your post-op follow-up visit. According to the U.S. National Library of Medicine, it may take up to six weeks for you to fully recover from the surgery.
EATING AFTER SURGERY
If you have had your gallbladder removed, you may be wondering about foods you can and cannot eat. Here are some tips for returning to your normal diet after surgery.
Start by gradually adding small amounts of low-fat foods to your diet. Eat plenty of fruits, vegetables, and lean protein sources such as chicken or fish.
Avoid high-fat foods, fried foods, and foods high in sugar. After surgery, your fat calories should be no more than 30% of your diet. Instead, slowly incorporate high-fiber foods as you heal.
It may take a while for your stomach to adjust to eating solid foods again. Be patient with yourself and take it slow. If you experience any discomfort or pain, talk to your doctor.
A long-term diet after gallbladder removal should include lower-fat foods and high-fiber foods. For example, continue to eat plenty of whole grains, fruits, and vegetables.
GI ISSUES
General anesthesia and discomfort from a breathing tube may cause post-operative nausea. Some patients also experience vomiting. If the vomiting is severe, accompanied by other symptoms (such as abdominal pain or fever), or causes discomfort, contact your surgeon immediately. The doctor may need to evaluate you for post-op complications or may need to prescribe an anti-nausea medication.
Loose stool is another post-surgical symptom to expect. These loose bowel movements may last four to eight weeks and typically resolve without additional treatment.
WHAT ARE THE POTENTIAL RISKS AND COMPLICATIONS OF GALLBLADDER REMOVAL?
Gallbladder removal is generally considered a safe procedure with relatively low risks and complications. However, like any surgery, there are potential risks that should be considered before undergoing the procedure.
One of the most common risks associated with gallbladder removal is digestive issues.
When the gallbladder is removed, bile flows directly from the liver to the small intestine, which can cause digestive problems in some individuals. However, most people recover from these symptoms within a few weeks of the procedure.
It’s important to note that the gallbladder is not essential for healthy digestion, and many individuals do not experience significant issues post-surgery.
Some may notice occasional loose stool, but this is generally not a cause for concern and typically resolves over time. If you experience any new symptoms or changes in your bowel habits following the surgery, it is crucial to discuss these with your health care team. They can provide guidance and reassurance, helping you to manage and understand any changes in your digestive health.
Another potential risk of gallbladder removal is bile leakage. This can occur when bile leaks into the abdominal cavity, causing pain and swelling. In some cases, additional surgery may be required to repair the leakage.
Infection is also a possibility after gallbladder removal. Infection can occur at the site of the incision or in the abdomen. If you notice symptoms of infection, such as fever, chills, or redness and swelling around the incision site, it’s important to contact your doctor.
Early treatment can help prevent the infection from spreading and causing more serious complications.
In rare cases, the bile ducts or other organs may be damaged during surgery. This can lead to more serious complications, such as chronic digestive problems. However, the risk of this occurring is relatively low.
Before undergoing gallbladder removal surgery, it’s important to discuss the potential risks with your doctor and ask any questions you may have.
WHEN TO CALL YOUR DOCTOR OR 911
Seek immediate, emergency care and call 911 if you:
- Lose consciousness or pass out
- Have difficulty breathing or are short of breath
Call your doctor if you have:
- Your original symptoms from before surgery
- A high fever
- Aausea and cannot drink fluids
- Worsening or severe pain, even with medications
- Discharge, redness, warmth, or increasing swelling from the wound
- Red streaks around the incision
- Bright red blood soaking through the bandage
- Loose stitches or your incision opens
- Jaundice, or yellowing skin or eyes
- Dark urine or whiteish stools, or cannot pass stools or gas
- Signs of a potential blood clot
These could be signs of an infection or a gallbladder surgery complication
HOW DO I KNOW IF I NEED GALLBLADDER REMOVAL SURGERY?
If you have large, painful gallstones, your doctor may recommend surgery to remove your gallbladder.
Gallstones form when there is an imbalance in the substances that create bile in your liver, and they are typically made of the bile byproducts cholesterol or bilirubin. The bile byproducts form small, pebble-like deposits that build up in your gallbladder—hence, the name gallstones.
Most of the time, gallstones are too small for people to feel and notice them. However, if the gallstones become larger or block bile ducts, they can cause severe pain and other symptoms:
- Sudden and intense abdominal pain near the gallbladder (upper right of the abdomen)
- Pain between the shoulder blades or right shoulder
- Jaundice (yellow skin and eyes)
- Nausea and vomiting
- High fever and chills
Conditions Cholecystectomy Treats
A cholecystectomy, or surgical removal of the gallbladder, may be recommended for several medical conditions. Here are some of the primary reasons:
- Symptomatic Gallstones: Often referred to as cholelithiasis, these are gallstones in the gallbladder that cause pain or other symptoms.
- Bile Duct Stones: Known as choledocholithiasis, this occurs when gallstones move into the bile duct, potentially leading to blockages and other complications.
- Gallbladder Inflammation: Cholecystitis is the inflammation of the gallbladder, which can cause severe pain and infection.
- Large Gallbladder Polyps: These polyps have the potential to become cancerous if they grow large enough.
- Pancreatitis: In some cases, gallstones can lead to inflammation of the pancreas, known as pancreatitis, necessitating gallbladder removal.
- Gallbladder Cancer Concerns: Suspicion or early findings of cancer in the gallbladder may also prompt the need for a cholecystectomy.
Each of these conditions can lead to significant discomfort and potential complications, making surgical intervention a critical option.
GALLSTONE RISK FACTORS
Like most medical conditions, some factors may increase your risk of painful gallstones. Some who have a higher risk of needing gallbladder surgery include:
- Females
- Pregnant women
- Overweight or obese people
- Those with a high-fat, high-cholesterol, and low-fiber diet
- Those with a family history of gallstones
- Those with liver disease
SCHEDULE A CONSULTATION FOR GALLBLADDER REMOVAL IN TENNESSEE
Are you worried you may have gallstones or be at high risk? Are you considering surgical removal of your gallbladder? Contact The Surgical Clinic for more information on this common procedure. Visit our locations page to learn about a clinic near you that benefits from board-certified providers with years of experience.
General surgeons in Greater Nashville

Dr. John Boskind
General Surgeon
Summit

Dr. Mark Cooper
General Surgeon
Downtown

Dr. Patrick Davis
General Surgeon
Southern Hills

Dr. Alex Fruin
General Surgeon
Summit

Dr. Mark Hinson
General Surgeon
Columbia

Dr. George Lynch
General Surgeon
Downtown Nashville

Dr. Clinton Marlar
General Surgeon
Skyline

Dr. James McDowell
General Surgeon
Downtown Nashville

Dr. Willie Melvin
General Surgeon
Smyrna

Dr. Chad Moss
General Surgeon
Columbia

Dr. William Polk
General Surgeon
Downtown

Dr. Drew Reynolds
General Surgeon
St. Thomas West

Dr. Joshua Taylor
General Surgeon
Smyrna

Dr. Davidson Oxley
General Surgeon
VIEW PROFILE

Dr. Tyson Thomas
General Surgeon
St. Thomas West

Dr. John Valentine
General Surgeon
Hendersonville

Dr. Tyler Watson
General Surgeon
Summit Clinic

Dr. Patrick Wolf
General Surgeon
St. Thomas West

