Referrals
Happy Holidays!
Words cannot express our gratitude for entrusting your patients to us with your referrals. We constantly strive to reach new heights with every procedure we perform, from the most common to the most complex.
We’ve compiled a few of our latest surgical advances as a resource for you to see what we’re able to offer your patients. Take a look around & let us know if you have any questions.
Advanced Surgical Techniques
Additional Info
Learn more about other procedures we offer by clicking the tabs below.
What is TIF for GERD?
TIF | Transoral Incisionless Fundoplication
Why is it better than alternatives?
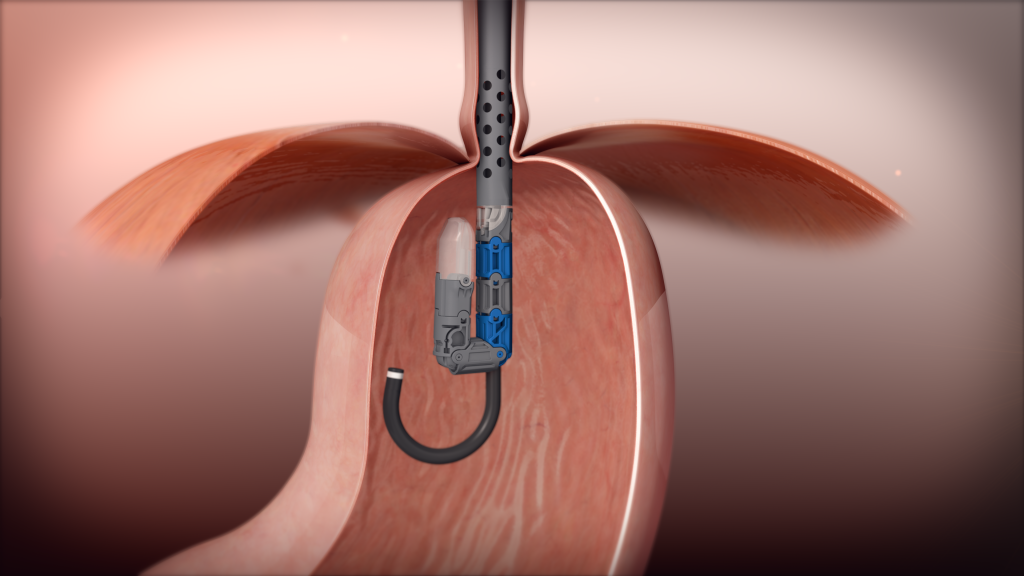
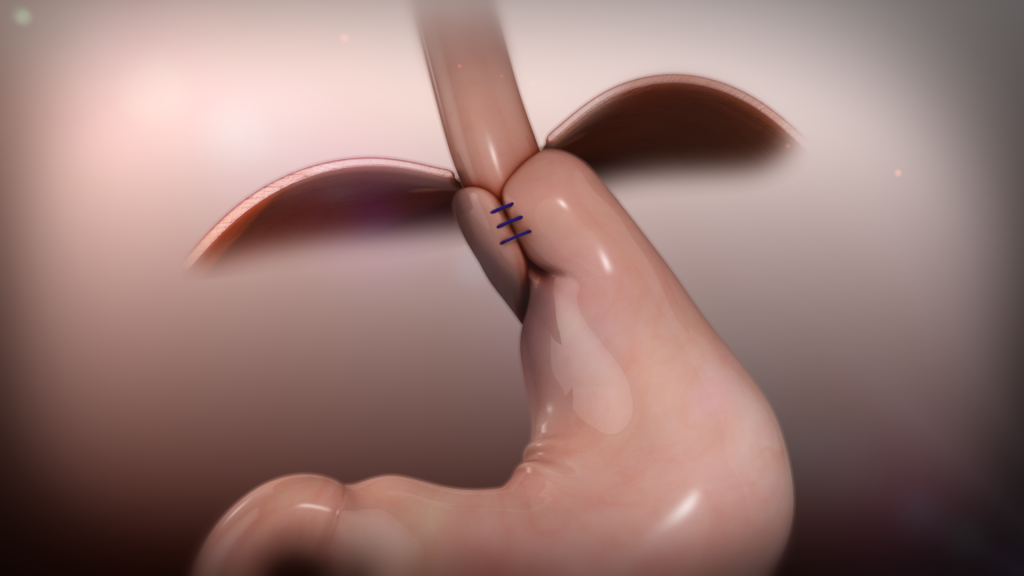
 TIF is an acronym, transoral incisionless fundoplication, and the advantage is that it is ‘surgery from within’ performed through the mouth, not through an incision. TIF procedure with the EsophyX device is a simple intervention that repairs the gastroesophageal valve, the root cause of GERD. The TIF procedure reconstructs the valve between the esophagus and the stomach to prevent reflux.
TIF is an acronym, transoral incisionless fundoplication, and the advantage is that it is ‘surgery from within’ performed through the mouth, not through an incision. TIF procedure with the EsophyX device is a simple intervention that repairs the gastroesophageal valve, the root cause of GERD. The TIF procedure reconstructs the valve between the esophagus and the stomach to prevent reflux.
- The FDA approved this device and procedure in 2007.
- Minimally invasive: Fast recovery
- Restores valve to natural state: Maintain normal bodily functions
- No incisions: No scars
- No metal implant: No need to remove foreign object
- No dissection of stomach: No scar tissue
Clinical studies show that at three years after the TIF procedure:
- 70% were able to completely stop PPI therapy
- 87% of patients reported reflux esophagitis healed
- 91% of patients reported elimination of troublesome regurgitation
Managing thyroid nodules
THYROID NODULE RFA
*Radio-Frequency Ablation
There is a non-surgical treatment available – with thyroid nodule RFA!
This is a new treatment being offered that avoids the need for surgery. This means you can keep the majority of your thyroid. There is much less risk of complication when compared to surgery.
Through an outpatient procedure, often with light sedation, nodules can be ablated (burned) with a needle device to cause them to shrink and destroy the tissue within the nodule that could turn cancerous. Typically one treatment is all that is needed for a nodule.
The benefits include:
- Outpatient procedure
- NO surgery. NO general anesthesia.
- Less risk of causing damage to surrounding thyroid or need for thyroid replacement hormone medications
- Keep your normal thyroid tissue
- Avoid possible complications of surgery
Dr. Joshua Taylor, MD completed his medical degree at Johns Hopkins University School of Medicine. His residency training was done at Vanderbilt Medical Center.
Dr. Joshua Taylor performs thyroid RFA for benign nodules in Smyrna, TN.
Advanced Hemorhoid Removal
HAL-RAR
HEMORRHOIDAL ARTERY LIGATION AND RECTAL ANAL REPAIR (HAL RAR)
This procedure is a slightly more invasive procedure, but it is highly effective at addressing the root cause of hemorrhoids. During this procedure, a miniature doppler radar is inserted into the anus and slowly rotated to identify the largest hemorrhoids. Once identified, a surgeon will suture off the arteries and cut off the blood flow.
With the blood flow cut off, the hemorrhoids will immediately shrink and disappear.
If a patient has more advanced hemorrhoids, or prolasped piles in the anal canal, Dr. Melvin can perform recto anal repair (RAR) to pull the prolapses back into place with sutures.
e-TEP Hernia Repair
Extended Totally Extraperitoneal Repair (eTEP)
One of the more prevalent procedures performed by General Surgeons are hernia surgeries. As you know, not all hernias are the same
And the term is not homogeneous. Hernias come in different sizes and locations. Hernias can be initial presentations (primary), or they may have been repaired before (recurrent). The goal of hernia surgery is to apply the basic tenets of hernia repair, close the hole and reinforce the repair. Through the advancement in technology we can perform complex abdominal wall reconstructions and hernia repair through smaller and smaller incisions. We have two state of the art fourth generation surgical robots that allow us to perform these complex surgeries.
Currently the most advanced hernia surgery performed is known as the eTEP hernia surgery.
This approach allows for repair of the hernia while working directly in the musculature layer to repair the hernia and avoid entry into the peritoneum. For patients with multiple prior surgeries or repairs this allows for avoidance of the potential for bowel injuries from prior scar tissue, we then are able to place the mesh material away from the viscera to prevent future issues of scaring to the mesh. We performed our first eTEP in December 2017, since that time we have performed over 100 such cases. This minimally invasive approach used in conjunction with our ESR (early surgical recovery) program, we can minimize post op pain and therefore minimize the need for narcotic use post operatively (reducing ME-morphine equivalence). With less pain and the need for less narcotic pain medication, patients can resume normal activity and return to normal function quicker.
Contact our office for your patient’s consultation to be evaluated for this exciting, new procedure.
Sending a referral?

Master Surgeons in Hernia Surgery
Congratulations to Dr. Willie Melvin & Dr. Joshua Taylor
Hernia Surgeons of Excellence in Hernia Surgery
Congratulations to Dr. Melvin and Dr. Taylor on achieving an SRC accreditation as a Master Surgeon in Hernia Surgery and Surgeon of Excellence in Hernia Surgery at Center of Excellence, TriStar StoneCrest Medical Center.
Surgical Review Corporation (SRC)
SRC is a nonprofit, patient safety organization. They accredit the top facilities, surgeons and medical professionals worldwide that meet proven standards.
