When it comes to your health, nothing holds more power than prevention. That is especially true when it comes to thyroid health. Unfortunately, there are a variety of health risks associated with this tiny gland, including thyroid cancer, which affects over 50,000 people annually.
The occurrence of thyroid cancer has experienced a growth of over two-fold since the 1970s, emerging as the swiftest expanding cancer diagnosis within the United States. It is the fourth most prevalent cancer among women, affecting females three times more frequently than males. But thyroid cancer can strike anyone and even hits the younger population more compared to other cancers.
That is why it’s essential to recognize September as Thyroid Cancer Awareness Month, a dedicated time to foster awareness about thyroid cancer to facilitate early detection, promote high-quality care following expert guidelines, and intensify research efforts toward finding effective treatments for all forms of thyroid cancer.
Here at The Surgical Clinic, our surgical oncologists want to help inform and educate you in honor of Thyroid Cancer Awareness Month. This article is your ultimate guide to everything you need to know about your thyroid and thyroid-related problems, including thyroid cancer.
THYROID BASICS 101: THE THYROIDS ANATOMY AND PURPOSE
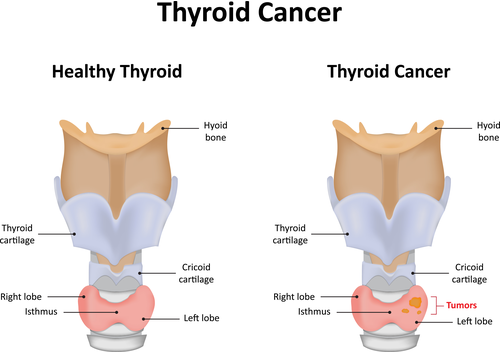
Before we discuss thyroid cancer, it’s important to understand what the thyroid is, what it does, and what other health issues an unhealthy thyroid can potentially influence.
What is The Thyroid?
The thyroid is a small butterfly-shaped gland located just below your Adam’s apple. You can’t see it or feel it, but it’s a vital part of your body’s endocrine system, which includes the pituitary, adrenal, and thyroid glands.
The thyroid’s influence is felt all throughout your body and plays a crucial role in maintaining your body’s balance and overall well-being. Together, this system forms a network that guides growth, development, and hormone production.
What Does the Thyroid Do?
The thyroid gland’s primary goal is the production of two hormones that influence everything from energy use and oxygen consumption to heart rate and body weight. These hormones, called T-3 and T-4, also regulate cholesterol levels, body temperature, and women’s menstrual cycles.
The thyroid’s role also extends to growth and development, ensuring proper brain and bone growth, especially in children. It also communicates with the pituitary to determine your body’s required levels of T-3 and T-4.
The thyroid might operate quietly in the background, but its contributions to your health are significant. As we discuss thyroid problems and thyroid cancer a little further down, you’ll gain a deeper understanding of the thyroid’s function and vulnerabilities.
SIGNS YOUR THYROID ISN’T HEALTHY
The signs of an unhealthy thyroid often exhibit a distinct pattern. These symptoms are rooted in the thyroid’s role in regulating various bodily functions through hormone secretion.
While some of these symptoms might overlap with other health concerns, their combination and persistence can signify thyroid dysfunction.
There are at least 20 signs your thyroid isn’t working right, but here are the most common indicators that your thyroid might not be functioning properly:
- Unexplained weight changes, gain or loss
- Persistent fatigue
- Hair loss
- Irregular menstrual cycles
- Dry skin and brittle nails
- Sensitivity to cold or heat
- Mood swings
- Muscle weakness and aches
(It’s important to note that the symptoms above are of thyroid dysfunction, not necessarily thyroid cancer. We will discuss thyroid cancer symptoms a little further down._
THYROID RELATED HEALTH PROBLEMS
Thyroid cancer isn’t the only thyroid-related medical issue. In fact, thyroid cancer is much less common than other thyroid-related health problems, such as having an overactive or underactive thyroid.
Here are some health problems that could be linked to thyroid dysfunction:
Hypothyroidism
An underactive thyroid, or hypothyroidism, occurs when the thyroid gland fails to produce sufficient hormones. This can lead to symptoms such as fatigue, weight gain, cold sensitivity, and sluggishness.
Hyperthyroidism
On the other end of the spectrum, hyperthyroidism is characterized by an overactive thyroid gland, resulting in an excess of thyroid hormones. This can cause symptoms like weight loss, rapid heartbeat, anxiety, and heat sensitivity.
Goiter
A goiter is an enlarged thyroid gland that can develop due to both hypothyroidism and hyperthyroidism. It can cause swelling in the neck and throat, leading to discomfort and breathing difficulties.
Thyroid Nodules
Thyroid nodules are abnormal growths within the thyroid gland. While most nodules are non-cancerous, some can lead to hyperthyroidism or, in rare cases, thyroid cancer.
Hashimoto’s Thyroiditis
This autoimmune disorder targets the thyroid, leading to inflammation and gradual destruction of the gland. Hashimoto’s can cause hypothyroidism and result in symptoms like fatigue, depression, and muscle weakness.
Graves’ Disease
Another autoimmune condition, Graves’ disease, causes the thyroid to become overactive. It often leads to hyperthyroidism and may trigger symptoms such as weight loss, bulging eyes, and mood swings.
Thyroiditis
Thyroiditis refers to inflammation of the thyroid gland, which can be caused by various factors. It can result in temporary hyperthyroidism followed by hypothyroidism as the inflammation subsides.
Thyroid Cancer
Though relatively rare, thyroid cancer can occur in the thyroid gland’s cells. Early detection and treatment are crucial for managing this condition effectively.
Because September is Thyroid Cancer Awareness Month, we want to deep dive into the understanding of this disease. The rest of this blog is dedicated to everything you need to know about thyroid cancer.
EVERYTHING YOU NEED TO KNOW ABOUT THYROID CANCER
Thyroid cancer originates in the thyroid gland and, like other cancers, develops when cells begin to change or mutate.
What sets thyroid cancer apart is its tendency to appear in a younger demographic compared to many other adult cancers. The average age of a thyroid cancer diagnosis is 51. Another interesting fact about thyroid cancer is that it is significantly more prevalent in women, with around three times more cases reported in women than in men. Racial differences also come into play, with approximately 70% more occurrences in White individuals compared to their Black counterparts, who exhibit the lowest incidence rate.
Although not as common as some other cancer types and often treatable, especially when caught early, thyroid cancer is still a serious and often deadly cancer that affects tens of thousands of people annually. According to The American Cancer Society, it’s projected that there will be about 43,720 new cases of thyroid cancer in the United States in 2023. Of those diagnoses, about 2,120 deaths are anticipated.
Up until recently, the rate of new thyroid cancer cases had been experiencing a significant surge, surpassing the incidence growth of any other cancer in the U.S. Researchers believe this was primarily driven by heightened detection during imaging procedures such as CT or MRI scans, which were conducted for other medical concerns. However, recent years have brought about a notable shift.
With the adoption of more rigorous diagnostic criteria, the incidence rate of thyroid cancer has declined, with an annual decrease of approximately 2%. Cancer experts believe this decline is partially due to the evolving understanding and approaches to the diagnosis and management of thyroid cancer, reflecting the medical community’s commitment to precision and informed care.
THYROID CANCER CAUSES AND RISK FACTORS
Thyroid cancer’s origins are influenced by factors that range from things out of your control (such as age, gender, and race) to things you do have some control over, such as environmental factors and lifestyle choices.
According to the National Cancer Institute, individuals with the following risk factors are more at risk of developing a type of thyroid cancer:
- Anyone between the ages of 25 and 65.
- A family history of thyroid disease or thyroid cancer.
- Having an existing thyroid condition.
- Thyroiditis (inflammation of your thyroid gland).
- Enlarged thyroid (goiter).
- Obesity (high body mass index).
- Low iodine intake.
- Significant exposure to radiation (especially during childhood.)
- Lifestyle choices such as smoking and exposure to certain chemicals.
Of those risks, a family history of thyroid cancer and significant radiation exposure are believed to be the two main risk factors for thyroid cancer.
Other risk factors include gender, ethnicity, and genetic conditions and mutations that cause endocrine diseases, such as multiple endocrine neoplasia type 2A (MEN2A) or type 2B (MEN2B) syndrome.
You can read more about these conditions on the National Cancer Institute’s website.
SYMPTOMS AND WARNING SIGNS OF THYROID CANCER
Thyroid cancer may present a range of symptoms, while some individuals may not experience any symptoms at all. Symptoms can vary widely, and while one person may notice changes, another might not be aware of any abnormalities.
- A lump or swelling in the front of the neck
- Hoarseness or voice changes
- Difficulty swallowing or breathing
- Pain or discomfort in the neck
- Persistent cough
- Throat or neck nodules
- Changes in voice pitch
(It is also important to note that just because you are experiencing symptoms does not necessarily indicate thyroid cancer. Still, they shouldn’t be ignored. If you begin to experience any of these warning signs (especially if you have any of the risk factors discussed), please call one of our general surgeons at The Surgical Clinic.)
THE FOUR TYPES OF THYROID CANCER
Thyroid cancer manifests in several distinct forms, each with its unique characteristics. Proper diagnosis, personalized treatment, and ongoing monitoring are vital in addressing these variations effectively.
- Papilary: Papillary thyroid cancer is the most common form of thyroid cancer. It grows slowly but may spread to lymph nodes on the neck.
- Follicular: Follicular cancer is the second most common form of thyroid cancer. It grows slowly and is found more in places with high iodine deficiencies. This is also one of the easiest types of thyroid cancer to treat.
- Medullary: Medullary is a less common form and is usually hereditary. It is more likely to spread to lymph nodes than papillary thyroid cancer, warranting vigilant observation.
- Anaplastic: Anaplastic thyroid cancer, though rarer, showcases an aggressive nature. Its rapid growth and extensive spread underlines its significant risk and urgency of management.
THE 4 STAGES OF THYROID CANCER
Thyroid cancer follows distinct stages that provide a clear picture of its development. These stages indicate how far the cancer has spread and aid in shaping the proper treatment approach.
Stage I:
In the initial stage of thyroid cancer, the malignancy is confined to the thyroid gland and has not extended beyond its boundaries. This stage is often characterized by smaller tumor sizes.
Stage II:
At this stage, thyroid cancer might still be limited to the thyroid gland, but tumor sizes may vary. Lymph node involvement in the neck might also be observed.
Stage III:
Thyroid cancer has now begun to spread beyond the thyroid gland and potentially invades nearby structures or lymph nodes. Tumor sizes may vary further.
Stage IV:
In the advanced stage of thyroid cancer, the malignancy may have spread to distant sites within the body, such as the lungs or bones. The size of the tumor and the extent of spread are significant factors in this stage.
Can Thyroid Cancer Spread?
As with many cancers, thyroid cancer can potentially spread to other parts of the body, known as metastasis. The likelihood of metastasis typically increases as the cancer progresses to higher stages.
Common sites of spread include:
- Lymph nodes in the neck
- The lungs
- Bones
Thyroid cancer can potentially spread to other areas of the body. It’s also possible for thyroid cancer to metastasize to the liver, brain, and other distant organs. However, metastasis to these organs is less common.
Determining whether thyroid cancer has spread involves a comprehensive approach to diagnosis. Medical professionals employ various imaging techniques, including ultrasound, CT scans, MRI scans, and radioactive iodine scans. These methods help visualize the extent of cancer’s reach beyond the thyroid gland.
HOW THYROID CANCER IS DIAGNOSED
Accurate diagnosis of thyroid cancer involves a multi-faceted process that draws on various diagnostic tools. Typically, several of the below methods are applied when diagnosing thyroid cancer. Here are so common ways thyroid cancer is diagnosed:
- Medical Evaluation: The first thing your doctor will likely do is perform a comprehensive medical evaluation, where your medical history and potential risk factors are examined. This evaluation aids in identifying any symptoms, family history, or previous medical conditions that might contribute to a better understanding of your thyroid health.
- Physical Examination: A physical examination follows, where a physician examines your neck for any abnormalities or signs of thyroid irregularities. This step often includes palpation of the thyroid gland to detect any nodules or growths.
- Imaging: Imaging is typically the next step in thyroid cancer diagnosis. Techniques like ultrasound, CT scans, and MRI scans provide detailed visualizations of the thyroid and surrounding structures. These images help determine the size, location, and characteristics of any potential thyroid nodules or tumors.
- Biopsy: If suspicious nodules are identified, a biopsy may be performed. A fine-needle aspiration biopsy involves extracting a small sample from the nodule for laboratory analysis. This procedure helps determine whether the nodule is cancerous or benign.
- Blood Tests: Blood tests, including thyroid function tests, measure hormone levels in your blood. While not diagnostic of cancer itself, abnormal hormone levels can provide insights into thyroid function and potential irregularities.
- Genetic Testing: Genetic testing may be recommended in some instances, especially for medullary thyroid cancer. Genetic analysis can identify specific mutations associated with thyroid cancer, aiding diagnosis and treatment planning.
HOW SERIOUS IS THYROID CANCER?
Thyroid cancer’s seriousness can vary widely based on several factors, including the type of cancer, its stage, and individual characteristics. However, most patients with thyroid cancer have an excellent prognosis and can be treated effectively.
In fact, the success rate of treating thyroid cancer is extremely high, with over 95% of patients living for more than five years. Following proper treatment, most patients can enjoy a normal lifespan and maintain their quality of life without significant compromises.
While many cases of thyroid cancer have favorable outcomes, it’s still important to recognize the potential for complications and the significance of early detection and treatment. If left untreated or not effectively managed, thyroid cancer can lead to a range of difficulties.
Some complications associated with thyroid cancer include:
- Spreading and metastasizing
- Breathing and swallowing difficulties
- Hormonal imbalances
- Recurrent of persistent cancer
- Side effects of treatment like fatigue, pain, or damage to nearby tissue
- Emotional and psychological impact
TREATMENT FOR THYROID CANCER
Thyroid cancer treatment decisions are best made in consultation with a medical team specializing in thyroid health and thyroid surgery. Tailoring treatment to the specific type and stage of thyroid cancer, along with individual health factors, ensures the most effective and personalized approach to managing the disease.
Surgical removal of the thyroid gland, known as a thyroidectomy, by an oncology surgeon is the most common treatment for thyroid cancer. The extent of surgery may vary based on the cancer’s type and stage. We will discuss types of thyroid cancer surgery in depth next.
First, here are other treatment modalities that might be considered or used in conjunction with thyroid surgery:
- Radioactive Iodine Therapy: This therapy involves taking a radioactive form of iodine, which is absorbed by thyroid cells. The radiation helps destroy any remaining thyroid tissue or cancer cells after surgery.
- Thyroid Hormone Therapy: Patients often take synthetic thyroid hormone medication to suppress the production of thyroid-stimulating hormone (TSH), which can stimulate the growth of any remaining thyroid cells.
- External Beam Radiation Therapy: This treatment uses focused external radiation to target and shrink thyroid cancer cells. It’s particularly useful for cancer that has spread to nearby structures.
- Targeted Therapy: Some advanced cases of thyroid cancer may benefit from targeted therapies that specifically target cancer cells’ growth signals.
- Chemotherapy: While less common for thyroid cancer, chemotherapy may be used in certain aggressive cases or when other treatments are ineffective.
- Clinical Trials: Participation in clinical trials offers access to experimental treatments that may show promise in treating thyroid cancer.
- Supportive Care: Complementary therapies, nutritional support, pain management, and counseling can play a crucial role in supporting overall well-being during treatment.
EVERYTHING YOU NEED TO KNOW ABOUT THYROID CANCER SURGERY
Most people with thyroid cancer choose to have thyroid cancer surgery. The surgical approach required can differ significantly, depending on the type and stage of the cancer being treated.
In this section, we will discuss your options for thyroid cancer surgery and what to expect before, during, and after surgery.
TYPES OF THYROID CANCER SURGERY
Lobectomy
A lobectomy removes the lobe containing the cancer. It is best for thyroid cancers that are small and show no signs of having spread to other parts of the body. After a lobectomy, patients typically don’t need thyroid hormone pills since the whole thyroid is not removed. However, leaving part of the thyroid can cause issues with cancer recurrence tests.
Thyroidectomy
In contrast to a lobectomy, a thyroidectomy removes the whole thyroid gland. Most surgeons perform a thyroidectomy through a small incision at the bottom of the neck, leaving a scar that fades over time.
Because the surgeon removes the entire thyroid, patients will need to take hormone pills. On the plus side, doctors can easily test for recurrence using radioiodine scans and thyroglobulin blood tests.
Transoral and Parathyroid Scarless Surgery
Most people do not want scars after surgery. Thankfully, transoral and parathyroid surgery leaves no scars. The surgeon makes three incisions in the lower lip and uses special instruments that pass under the skin to access the thyroid for either partial or full removal.
Lymph Node Removal
For advanced thyroid cancers that have spread to nearby lymph nodes in the neck, a surgeon will remove those lymph nodes. Typically, medullary thyroid cancer and anaplastic cancer require lymph node removal.
WHAT HAPPENS BEFORE, DURING, AND AFTER THYROID CANCER SURGERY
The prospect of surgery, especially for thyroid cancer, can be an anxiety-inducing experience. Understanding the process from start to finish, including its invasiveness, expected recovery time, and potential challenges, can provide a sense of reassurance and empowerment during this pivotal moment in your journey to wellness.
Before Thyroid Cancer Surgery
As you gear up for thyroid cancer surgery, your surgical team will guide you through the necessary preparations. The personalized instructions your surgeon advises are crucial for ensuring the success of the surgery, a smoother recovery, and your overall well-being.
This may involve adjusting medications like aspirin or other blood thinners, along with certain herbs and supplements. Additionally, you’ll be instructed not to eat or drink anything for around 12 hours before the scheduled surgery.
Adhering to the pre-surgery instructions is pivotal in minimizing potential complications and optimizing the surgical process. By diligently following these pre-surgery guidelines, you actively contribute to a smoother surgical experience and set the stage for a smoother recovery.
During Thyroid Surgery
First, you will be administered an IV to give your body the fluids and medication needed for the procedure. You’ll then be given general anesthesia to keep you asleep and pain-free throughout the surgery.
Once asleep, an incision is made at the bottom of your neck along a crease in your skin. The surgeon will decide how much of the thyroid gland is removed. This will depend on how far the cancer has spread. As a result, your surgeon may not know how much to remove until the day of your surgery.
After the thyroid has been removed, the incision is closed with sutures, and you will be moved into a recovery room.
Post Thyroid Surgery
Following thyroid surgery, your recovery process will vary based on the extent of the procedure and your individual response. In some cases, you can return home on the same day as the surgery, while in others, a short hospital stay may be recommended.
For those who can go home the same day, you’ll be closely monitored to ensure your condition is stable and any immediate post-operative concerns are addressed. The medical team will provide clear post-operative instructions to facilitate your recovery at home. These instructions will include things such as managing pain, taking prescribed medications, and watching for any signs of complications.
In situations where a brief hospital stay is advised, typically ranging from one to several days, this allows the medical team to closely monitor your recovery progress. During this time, they can address any potential postoperative challenges and ensure you are on the path to a safe and successful recovery.
Your medical team will assess factors such as pain management, swallowing, voice quality, and the functioning of the parathyroid glands before determining the appropriate time for you to return home.
Risks Associated with Thyroid Cancer Surgery
While generally considered safe and effective, like any medical procedure, thyroid cancer surgery carries its own set of potential risks and complications that patients should be aware of.
Some potential side effects of this procedure may include:
- Bleeding: There is a small risk of bleeding during or after surgery, which might require additional treatment.
- Infection: Surgery could lead to infection at the surgical site, requiring treatment with antibiotics.
- Voice Nerve Damage: There’s a slight chance of temporary or permanent hoarseness due to nearby nerve involvement.
- Parathyroid Issues: The nearby parathyroid glands might be affected, potentially causing calcium level changes.
While these risks exist, they are rare, especially when performed by board-certified surgeons that specialize in thyroid cancer surgeries. At The Surgical Clinic, you are in excellent hands with our board-certified surgeons. They are experts in thyroid function and performing thyroid surgeries.
WHY THYROID CANCER AWARENESS MONTH IS IMPORTANT
Thyroid Cancer Awareness Month in September holds a significant place in our healthcare calendar. It serves as a platform for change, casting a spotlight on the significance of early detection, the advancement of treatment methods, the cultivation of survivorship, the reduction of prevalence, and the stimulation of research efforts.
By delivering essential knowledge, Thyroid Cancer Awareness Month empowers individuals to take charge of their well-being, contributing to the collective mission of mitigating the impact of thyroid cancer and fostering healthier communities and individuals.
Healthcare professionals aren’t the only ones that can contribute to this important awareness month. You can also make a positive impact by encouraging those around you to stay informed about thyroid health.
To increase awareness, you can share educational resources such as this blog with family and friends. Additionally, consider getting screened if you’re at risk or due for a check-up. Early detection can be a lifesaver.
You could also support organizations that focus on thyroid cancer research and advocacy. Donations, participation in fundraising events, or volunteering your time can all be meaningful ways to contribute.
When we come together and take these steps, we’re uniting to create positive changes, building understanding, and working towards lessening thyroid cancer’s impact on individuals and communities. Together, we can truly make a difference.
THYROID SURGERY IN NASHVILLE TENNESSEE
If you feel a lump in your throat, are experiencing pain in the neck, or notice any other common signs of thyroid cancer, we urge you to contact one of our general or oncology surgeons at The Surgical Clinic in Nashville, Tennessee, who specialize in thyroid/endocrine surgery.
Thyroid Surgeons in Tennessee
If you feel a lump in your throat or are experiencing pain in the neck, we urge you to contact one of our general surgeons at The Surgical Clinic who specialize in thyroid/endocrine surgery.
General surgeons in Greater Nashville

Dr. John Boskind
General Surgeon
MT. JULIET

Dr. Mariana Chavez
General Surgeon
Downtown

Dr. Patrick Davis
General Surgeon
SOUTHERN HILLS

Dr. Gretchen Edwards
General Surgeon
DOWNTOWN

Dr. Alex Fruin
General Surgeon
MT. JULIET

Dr. James Griscom
General Surgeon
NASHVILLE

Dr. Mark Hinson
General Surgeon
COLUMBIA

Dr. George Lynch
General Surgeon
NASHVILLE

Dr. Clinton Marlar
General Surgeon
SKYLINE

Dr. Willie Melvin
General Surgeon
SMYRNA

Dr. Chad Moss
General Surgeon
COLUMBIA

Dr. William Polk
General Surgeon
NASHVILLE

Dr. Drew Reynolds
General Surgeon
SAINT THOMAS WEST

Dr. Joshua Taylor
General Surgeon
SMYRNA

Dr. Davidson Oxley
General Surgeon
COLUMBIA

Dr. Tyson Thomas
General Surgeon
SAINT THOMAS WEST

Dr. John Valentine
General Surgeon
HENDERSONVILLE

Dr. Patrick Wolf
General Surgeon
SAINT THOMAS WOLF

