WHAT IS RAYNAUD’S DISEASE?
AKA Raynaud phenomenon or Raynaud syndrome. There’s no cure for Raynaud’s disease, but you can manage it to help prevent attacks.
What triggers Raynaud’s disease?
→ Cold
→ Stress
→ Caffeine
→ Smoking
→ Repetitive movements
→ Certain medicines, such as beta-blockers, migraine medicine, birth control pills, and others
→ Injury
→ Emotions
Other triggers and causes:
Raynaud’s disease can be set off by more than just a chilly breeze or a case of nerves. It can also be linked to underlying health conditions, especially autoimmune or connective tissue diseases, scleroderma, lupus, rheumatoid arthritis, or Sjögren syndrome. Blood vessel disorders, like those that cause a buildup of fatty deposits or inflammation in the vessels of your hands and feet, may also play a role.
Physical factors can make things worse:
- Carpal tunnel syndrome (pressure on the main nerve to your hand) can make your hands extra sensitive to cold.
- Injuries, including fractures, surgery, or frostbite, can spark symptoms.
- Repeated actions or vibration from activities like long hours of typing, playing piano, or using tools like jackhammers can trigger attacks.
Lifestyle choices have a say, too. Smoking, which narrows blood vessels, increases your risk. Even certain medications, some used for high blood pressure, migraines, ADHD, cancer, or even over-the-counter cold remedies, can bring on Raynaud’s symptoms or make them worse.
It’s a mixed bag of triggers, but knowing what sets off your Raynaud’s can help you stay a step ahead.
Can air conditioning bring on Raynaud’s attacks?
Yes, air conditioning can trigger Raynaud’s attacks because even mild cold exposure, like stepping into a chilly, air-conditioned room, may cause blood vessels to constrict. If you’re sensitive, try setting your AC a bit warmer or keeping a cozy sweater or gloves handy to help keep your fingers and toes from getting too cold.
WHAT ARE THE SYMPTOMS OF RAYNAUD DISEASE?
What happens during an attack?
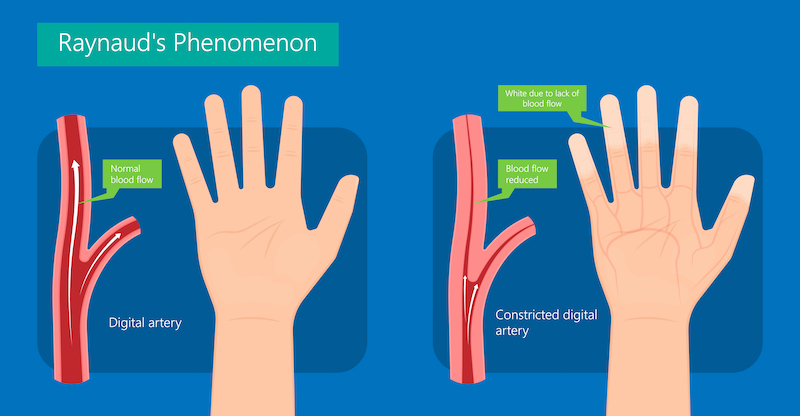
A Raynaud’s disease attack is often triggered by cold or stress. During an attack, blood vessels suddenly narrow (called vasospasm). This most often happens in fingers and toes. In rare cases, the nose, ears, nipples, or even tongue are affected. Narrowed blood vessels reduce the blood supply to the area. The area then turns white, blue, or red. The area may feel tingling, numb, or painful. As the attack passes, the blood vessels open. The affected area may turn bright red as it warms up, then returns to normal color.
For most people, Raynaud’s disease isn’t disabling, but it can certainly affect your quality of life. The severity and impact can vary; some experience only mild, occasional episodes, while others may find their daily activities interrupted by frequent or intense attacks. If you have other health conditions in addition to Raynaud’s, your experience may differ or require additional care.
How long does it take for blood flow to return after a Raynaud’s attack?
Blood flow doesn’t bounce back instantly; it can take anywhere from a few minutes to about 15 minutes for normal color and sensation to return, depending on how long the blood vessels remain narrowed. Warmth and movement can help speed things along, but patience (and some cozy mittens) is key.
WHEN SHOULD YOU SEE A DOCTOR FOR RAYNAUD’S DISEASE?
If you have Raynaud’s disease and notice sores, ulcers, or signs of infection on your fingers or toes, reach out to your healthcare provider as soon as possible. Wounds that don’t heal or get worse are a reason to seek medical advice right away.
You should also let your doctor know if:
- Your symptoms are severe or seem to be getting worse
- Attacks are happening more frequently or lasting longer than usual
- You find it difficult to perform daily activities because of Raynaud’s symptoms
- The color changes in your skin spread to other areas, like your nose or ears
Prompt attention can help prevent complications and ensure that you get the right treatment for your needs.
WHAT IS THE CAUSE OF RAYNAUD’S DISEASE?
With Raynaud disease, it’s believed that blood vessels in the affected areas respond too strongly to certain triggers, such as cold. This makes them narrow (called vasospasm) much more than in people without the disease. Experts don’t know what causes the blood vessels to react so strongly to certain triggers. In between attacks, the blood vessels are normal and healthy. Attacks don’t permanently damage the blood vessels. But they may thicken the artery walls.
In most cases, this thickening doesn’t cause long-term issues. However, in rare and more severe cases, especially with secondary Raynaud’s disease, repeated or prolonged reduction in blood flow can lead to complications. If blood flow is severely reduced, tissue damage can occur, sometimes resulting in skin sores or, very rarely, tissue death. In extreme, untreated instances, this might even require removal (amputation) of the affected area. Fortunately, these severe complications are uncommon, and most people with Raynaud’s disease never experience them.
In some cases, Raynaud’s disease happens along with another disease or condition. This is often a connective tissue disorder, such as lupus, scleroderma, or rheumatoid arthritis. This is called secondary Raynaud’s disease (as opposed to primary Raynaud’s disease discussed above) and may be more severe. If this is the case for you, you and your healthcare provider can discuss treatment for the underlying condition.
How does carpal tunnel syndrome relate to Raynaud’s disease?
Carpal tunnel syndrome can sometimes make Raynaud’s symptoms worse. This is because carpal tunnel syndrome puts pressure on the main nerve in your wrist, which can lead to numbness or tingling in your fingers and hands. If you already have Raynaud’s disease, the nerve irritation from carpal tunnel syndrome may make your hands even more sensitive to cold or trigger episodes more easily. If you notice these overlapping symptoms, talk with your healthcare provider—they can help you manage both conditions together.
WHAT BLOOD VESSEL DISEASES CAN CAUSE SECONDARY RAYNAUD’S DISEASE?
Certain blood vessel diseases can increase the chances of developing secondary Raynaud’s disease. These include:
- Atherosclerosis: This is when fatty deposits build up inside the blood vessels, making it harder for blood to flow. If the vessels supplying the hands and feet are affected, Raynaud’s symptoms may follow.
- Vasculitis: This is inflammation of the blood vessels, which can reduce blood flow to various parts of the body, including fingers and toes.
- Pulmonary hypertension: High blood pressure in the arteries of the lungs can also contribute to secondary Raynaud’s disease.
If you have a condition that affects your blood vessels, talk to your healthcare provider about your risks and ways to manage symptoms.
HOW DO CONNECTIVE TISSUE DISEASES CONTRIBUTE TO RAYNAUD’S DISEASE?
Connective tissue diseases, like scleroderma, lupus, rheumatoid arthritis, Ehlers-Danlos syndrome, or Sjögren syndrome, can increase the risk of developing Raynaud’s disease. These conditions may cause inflammation or changes in blood vessels, making them more likely to overreact to triggers like cold or stress. For example, scleroderma often thickens and hardens the skin and surrounding tissues, which can affect how blood flows to your fingers and toes. If you have any of these autoimmune or connective tissue disorders, your blood vessels are more likely to narrow suddenly, setting off a Raynaud’s attack.
WHAT ARE THE RISK FACTORS?
Who is at risk for primary Raynaud disease?
Some people are more likely than others to develop primary Raynaud’s disease. Here’s what bumps up your risk:
- Gender: Women are more likely to get Raynaud’s disease than men.
- Age: It often starts in your teens or young adulthood, most commonly between ages 15 and 30.
- Climate: Living in colder climates (think Minnesota winters, not Florida beaches) increases your risk.
- Family history: If you have a close family member (like a parent or sibling) with Raynaud’s disease, your chances go up.
Keep these risk factors in mind if you or someone close to you is experiencing symptoms.
→ Women are more likely to get Raynaud’s disease than men.
→ Younger people are at higher risk, usually ages 15 to 30.
→ Living in colder climates increases risk.
→ Having a family member with Raynaud’s disease increases your risk.
→ Underlying rheumatoid conditions may increase your risk.
WHAT ARE THE RISK FACTORS FOR SECONDARY RAYNAUD DISEASE?
Secondary Raynaud’s disease is often linked to other underlying health problems or specific exposures. Here are some factors that increase your risk:
→ Having certain autoimmune or connective tissue diseases, like scleroderma or lupus.
→ Working in jobs with repeated hand or finger vibration (think jackhammer operators, machinists, or anyone who uses vibrating tools regularly).
→ Exposure to chemicals, such as vinyl chloride.
→ Taking medicines that affect blood flow, including some used for migraines or high blood pressure.
→ Smoking or other forms of tobacco use, which can constrict blood vessels and make symptoms worse.
If you have one or more of these risk factors, talk with your healthcare provider about how to best manage your risk for secondary Raynaud’s disease.
HOW IS RAYNAUD’S DISEASE DIAGNOSED?
Your description of your symptoms, a health history, and a physical exam are often enough for a diagnosis. Blood tests and other tests may be done to see if any underlying conditions are present and rule out other problems.
HOW IS RAYNAUD’S DISEASE TREATED?
There is no known cure for Raynaud’s disease. But you can learn to manage symptoms and reduce the number and severity of attacks. For most people, avoiding triggers may be enough to limit attacks. Your healthcare provider may suggest the following:
→ Take safety steps to help prevent your hands and feet from losing circulation. This includes:
- Dressing warmly in cold weather.
- Wearing gloves or mittens when your hands may become cold, such as when you use the refrigerator or freezer.
- Avoiding stress and caffeine.
- Exercising regularly – this may reduce the number and severity of attacks.
- If you smoke, quitting may improve the condition – smoking causes your blood vessels to narrow and reduces blood flow.
→ Soak your hands or feet in warm (not hot) water. Do this at the first sign of an attack. Keep soaking until your skin color returns to normal.
MANAGING RAYNAUD’S DISEASE INDOORS
Living with Raynaud’s disease means being proactive—even inside your own home. Here are a few simple tips to help reduce your chances of an indoor attack:
→ Keep your feet warm by wearing socks, even around the house.
→ If you need to handle cold items, like food from the fridge or freezer, use gloves, mittens, or oven mitts to protect your fingers from sudden temperature changes.
→ During colder months, some people find it helpful to wear socks or mittens to bed to keep hands and feet cozy overnight.
→ Watch your indoor temperature—set your thermostat a little warmer if you start to notice symptoms, and avoid strong air conditioning that can trigger attacks. Insulated drinking glasses can also help keep your hands from getting chilled while enjoying a cold drink.
Simple steps like these can go a long way in helping you manage Raynaud’s disease indoors and keep symptoms at bay.
SUPPORT FOR PEOPLE LIVING WITH RAYNAUD’S DISEASE
Living with Raynaud’s disease can sometimes feel isolating, but you’re not alone. Several support groups and organizations exist for people affected by Raynaud’s disease and other vascular conditions. Connecting with others who share similar experiences can offer emotional support, practical tips, and answers to your questions.
Here are some ways to find support:
- Raynaud’s Association: This nonprofit offers resources, forums, and a supportive online community specifically for people with Raynaud’s disease.
- Scleroderma & Raynaud’s UK (SRUK): Provides information, helplines, and opportunities to connect with others living with Raynaud’s through online communities and local events.
- Social Media Groups: Many people find comfort and advice in Facebook groups dedicated to Raynaud’s disease. Just search “Raynaud’s support group” to find active online communities.
- Local Hospitals or Community Centers: Ask your healthcare provider if there are any support groups, workshops, or educational sessions in your area. Some hospitals host regular meetings for vascular health.
Support groups create opportunities to learn from others, share coping strategies, and find encouragement in managing daily challenges. Whether online or in person, finding your community can make all the difference as you navigate life with Raynaud’s disease.