What is Gallbladder Disease?
Gallbladder disease is a term used for several types of conditions that affect the body’s bile system. This system includes the liver, gallbladder, and bile ducts. If you’re wondering where your gallbladder is, it is located underneath your liver.
Your gallbladder’s main function is to store the bile produced by your liver. It also passes the bile through a duct that empties into the small intestine. Bile is used to help you digest fats in your small intestine. Sometimes, the bile hardens and forms small, solid particles that we call gallstones.
Types of Gallbladder Disease
Common health issues that can affect the gallbladder are:
Gallstones
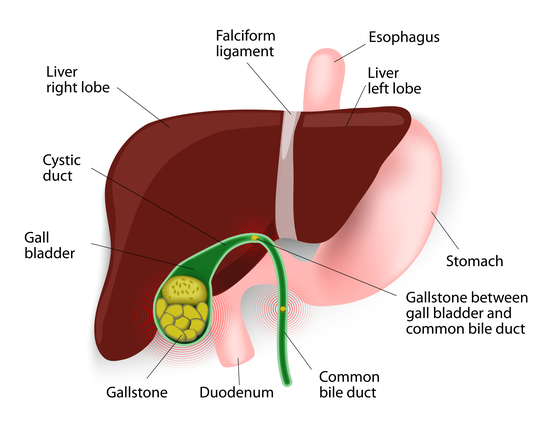
Gallbladder disease occurs when substances in the bile, such as cholesterol, bile salts, and calcium build up in the bile system. These substances develop gallstones that block the passageways to the gallbladder and bile ducts.
Gallstones can also form when the gallbladder doesn’t completely empty. And gallstones can range from the size of a small grain of sand to the size of a golf ball.
Types of Gallstones
There are two types of gallstones, cholesterol stones, and pigment stones. Cholesterol stones are the most common type and are typically larger. Pigment stones are smaller but usually more than one pass at a time.
Symptoms and Signs
Oftentimes gallstones do not cause any symptoms. However, as the gallstones grow larger, they can become trapped in an opening or duct inside the gallbladder. When this occurs, you may feel symptoms such as:
- Severe pain in the upper abdomen (gallbladder attacks)
- Pain in the back between the shoulder blades
- Nausea
- Vomiting
- Fever
- Jaundice – a yellowing of the skin or eyes
- Abdominal bloating
- Intolerance of fatty foods
- Belching or gas
- Indigestion
Each individual may experience symptoms differently. Anyone suffering severe pain should consult a doctor immediately.
What Symptoms Can Stones Lodged in the Common Bile Duct Cause?
Stones that become stuck in the common bile duct can trigger a range of symptoms, some of which are similar to those caused by gallbladder stones. Here are the key symptoms to watch for:
- Jaundice: A yellowish tint to the skin and eyes, due to bilirubin buildup.
- Changes in Urine and Stool: Urine may become unusually dark, while stools could appear lighter than normal.
- Cardiovascular Symptoms: Expect possible rapid heartbeat and a sudden drop in blood pressure.
- Systemic Symptoms: Fever, chills, nausea, and vomiting, combined with intense pain in the upper right abdomen.
Key Points:
- Jaundice: Indicates bile flow issues.
- Urine and Stool Variations: Reflect liver and bile duct issues.
- Heart and Blood Pressure: A direct response to pain and bile duct obstruction.
- Fever and Pain: Signals of an infection or significant blockage.
Understanding these symptoms can help you take timely action and seek medical help when necessary.
Cholecystitis
Cholecystitis is the most common type of gallbladder disease. This is a more severe gallstone blockage inside a biliary tract that can cause swelling in the gallbladder. It presents itself as either an acute or chronic inflammation of the gallbladder.
Acute cholecystitis
The main symptom of this acute gallbladder disease is a sudden sharp pain in the abdomen that may last 6 hours or longer. This is commonly referred to as a gallbladder attack. Gallbladder attacks cause pain in the upper right side of the abdomen.
Acute cholecystitis develops when stones or sludge block the duct, leading to inflammation. The pain is typically severe and constant—it doesn’t let up, and it can last for days. Often, this pain worsens when you take a deep breath, and may radiate to other areas such as the back, under the shoulder blades, or even behind the breastbone. About a third of those affected also experience fever and chills, which are not usually present in uncomplicated biliary colic. Nausea and vomiting are frequent companions, and the discomfort can be relentless.
Chronic cholecystitis
This chronic condition is the result of long-term inflammation in the gallbladder. This occurs when the gallbladder does not drain properly.
Symptoms include recurrent abdominal pain. Nausea and vomiting may also occur. Gallbladder inflammation can cause many serious complications like infection, tissue decay, and gallbladder tears.
Both forms of gallbladder inflammation can lead to critical complications. Seek medical attention immediately if a person shows any of the symptoms listed above.
What does a gallbladder attack feel like?
A gallbladder attack usually starts as a sudden pain that grows worse in the upper right or center of the body. This pain can also be located in the back between the shoulder blades or in the right shoulder. While some last minutes, other gallbladder attacks last hours. The fastest way to relieve gallbladder pain is to apply a heated compress, heating pad, hot water bottle, or warm wet towel to the area for 10-15 minutes. Magnesium supplements can also aid in the gallbladder emptying bile and ease spasms and pain.
Some people may experience additional signs and symptoms, such as:
- nausea and vomiting
- a fever
- slight yellowing of the skin
- or swelling in the abdomen
How Long Does a Gallbladder Attack Last?
A gallbladder attack will typically last anywhere between 15 minutes to several hours. Often, the pain can escalate to high levels and can radiate to the left side of the body and to the back. The pain may also come and go over time. Meals high in fat tend to aggravate gallbladder irritations, so reducing fat intake can be helpful.
How to Stop a Gallbladder Attack While It Is Happening:
While pain from a gallbladder attack can not be immediately stopped until the gallstone passes, there are actions to take to lessen the pain of gallbladder attacks. Some ways to treat a gallbladder attack while its happening includes:
- Over the counter pain medicine
- Warm compress to the abdomen
- Peppermint tea
Risk Factors for Gallbladder Disease
There are many risk factors for gallbladder disease. A few of the most common risks are associated with gender, age, obesity, and ethnicity. Gallbladder attacks often happen when a stone blocks a passageway in the gallbladder. Gallstones themselves form when substances in bile create hard particles that can range in size from a grain of sand to as large as a golf ball.
Women are generally at higher risk of developing gallstones than men, and this risk increases with age and the number of children a woman has had. Pregnancy is a particular risk factor for gallstone formation, but interestingly, breastfeeding can help reduce that risk. Additionally, women who use hormone replacement therapy are more likely to develop gallstones.
Other risks include:
- Sedentary lifestyles
- Fat and cholesterol-rich diets
- Family history of gallbladder disease
- Diabetes
- Blood disorders
- Liver disease
- Pregnancy
- Treatment for Gallbladder Disease
How Do Pregnancy, Breastfeeding, and Hormone Replacement Therapy Affect Gallstone Risk?
Certain life stages and hormonal changes can influence your chances of developing gallstones.
- Pregnancy: Expectant mothers face a higher risk of gallstone formation. This is due to hormonal shifts during pregnancy that make bile more likely to form solid particles, leading to blockages in the gallbladder.
- Number of Children: The risk for gallstones increases with the number of pregnancies. More pregnancies mean more repeated exposure to the hormonal changes that encourage gallstone development.
- Breastfeeding: On the bright side, breastfeeding appears to lower the risk of developing gallstones after pregnancy, as it helps the body regulate certain hormones and may aid in returning bile composition to normal.
- Hormone Replacement Therapy (HRT): Women taking HRT, such as postmenopausal estrogen therapy, are at increased risk for gallstones. This is because additional estrogen can contribute to the conditions that encourage gallstone formation.
If any of these factors apply to you, it’s especially important to monitor for gallbladder symptoms and discuss your risks with your healthcare provider.
How is Gallbladder Disease Diagnosed?
- Medical History and Physical Exam: Your healthcare provider will start by reviewing your medical history and conducting a physical examination to check for symptoms like abdominal pain or tenderness.
- Blood Tests: These help identify signs of infection, inflammation, and issues with liver function, which can indicate gallbladder problems.
- Imaging Techniques: Various imaging tests are used to visualize the gallbladder. Common methods include:
- Ultrasound: Often the first test performed, it uses sound waves to create images of the gallbladder and check for abnormalities like gallstones.
- CT Scan: Provides detailed cross-sectional images of the gallbladder and surrounding organs.
- HIDA Scan: Tracks the production and flow of bile from the liver to the small intestine, which can reveal blockages or functional issues.
- MRCP (Magnetic Resonance Cholangiopancreatography): A type of MRI that specifically focuses on the liver, gallbladder, bile ducts, and pancreas.
- Endoscopic Procedures: In some cases, an endoscopic test may be needed. Techniques like ERCP (Endoscopic Retrograde Cholangiopancreatography) allow doctors to examine and treat issues within the bile ducts.
By combining these diagnostic tools, healthcare providers can accurately diagnose and tailor treatment plans for gallbladder disease.
Prevention and Treatment
Lifestyle changes
Because low activity rates are one of the risk factors for gallbladder disease, daily lifestyle changes may help. If you do not have symptoms of gallbladder disease, these changes may even prevent symptoms. Lifestyle changes may include increasing physical activity or reducing unhealthy fats in your diet.
While it can be tempting to make dramatic changes to your diet, extreme dieting will hurt you more. In contrast, if you want a healthy diet, it is more about eating in balance. For example:
- Eat plenty of fruits and vegetables
- Buy whole grain breads and cereals
- Include legumes such as beans and peas in your meals
- Use healthy fats like olive oil
With this in mind, you can begin to prevent gallbladder disease on your own. However, if you have any questions, talk to your doctor. You can also ask a nutritionist, in addition to your doctor, about safe ways to manage your daily lifestyle and diet.
Medical treatment
The first episode of gallbladder inflammation is often treated with pain medications. Because the pain is often severe, prescription medications are needed.
The first episode of gallbladder inflammation is often treated with pain medications. Because the pain is often severe, prescription medications are needed.
In addition to pain control, the initial approach focuses on “resting” the gallbladder to help reduce inflammation. This typically includes:
- Fasting – You may be asked to avoid food and drink for a period of time, giving your gallbladder a chance to settle.
- Intravenous fluids – These help prevent dehydration while you’re not eating or drinking.
- Oxygen therapy – Sometimes provided, especially if you’re feeling unwell or have trouble breathing comfortably.
- Stronger pain relief – Medications such as meperidine (Demerol) or potent NSAIDs like ketorolac may be used for effective pain management.
- Antibiotics – If there are signs of infection (such as fever or an elevated white blood cell count), intravenous antibiotics can be started right away. Even without obvious infection, antibiotics may be added if symptoms don’t improve after 12 to 24 hours.
This combination of supportive care and medications aims to alleviate inflammation and control symptoms, while your care team monitors for any changes. If improvement is not seen, or if complications develop, further interventions may be considered.
Surgery
Surgery will be recommended to remove your gallbladder if you’ve experienced multiple episodes of inflammation. Gallbladder surgery continues to be the most effective method for treating gallbladder disease.
Surgeons often use a technique known as laparoscopy to remove the gallbladder. This involves making several small incisions through the abdominal wall and inserting a camera. Your abdomen is then inflated with gas, so the surgeon has more room to work. And then, the surgeon will remove your gallbladder through the incisions.
Laparoscopic surgery allows for faster recovery. This method is preferred for people who don’t have complications of significant gallbladder disease. Pain after gallbladder surgery is often caused by the gas put into the abdomen after surgery and will subside after 24-48 hours.
Laparoscopic vs. Open Cholecystectomy: What’s the Difference?
If you need your gallbladder removed, your surgeon will decide between two main surgical approaches: laparoscopic cholecystectomy and open cholecystectomy. Here’s what you should know about the differences.
- Laparoscopic Cholecystectomy is the more common and less invasive option. The surgeon makes several small incisions in your abdomen and inserts a thin camera (laparoscope) along with special instruments. Your abdomen is gently inflated with gas to create space to work. Most people recover faster, experience less postoperative pain, and go home the same day or after an overnight stay.
- Open Cholecystectomy involves a single, larger incision in the upper abdomen to directly access and remove the gallbladder. Surgeons may recommend this method if you have severe inflammation, scar tissue from previous surgery, or complications that make laparoscopy unsafe. Recovery usually takes longer—sometimes up to a week in the hospital—before you can return to regular activities.
In summary, whenever possible, laparoscopic surgery is preferred because it offers a quicker recovery and less discomfort. Open surgery is reserved for more complex cases when necessary.
If you need treatment for gallbladder disease, start by getting to know some of our surgeons who offer gallbladder surgery. See our general surgeon below who specialize in gallbladder surgery.
Schedule Your Appointment Today
If you are searching for relief from symptoms caused by gallbladder disease, contact The Surgical Clinic and schedule a consultation. Or visit one of our clinic locations in Nashville, Franklin, Gallatin, Hermitage, Mt. Juliet, Murfreesboro, and Smyrna, TN. If you experience repeating gallbladder attacks, medical intervention may be the best solution for your health.
General surgeons in Greater Nashville

Dr. John Boskind
General Surgeon
MT. JULIET

Dr. Mariana Chavez
General Surgeon
Downtown

Dr. Patrick Davis
General Surgeon
SOUTHERN HILLS

Dr. Gretchen Edwards
General Surgeon
DOWNTOWN

Dr. Alex Fruin
General Surgeon
MT. JULIET

Dr. James Griscom
General Surgeon
NASHVILLE

Dr. Mark Hinson
General Surgeon
COLUMBIA

Dr. George Lynch
General Surgeon
NASHVILLE

Dr. Clinton Marlar
General Surgeon
SKYLINE

Dr. Willie Melvin
General Surgeon
SMYRNA

Dr. Chad Moss
General Surgeon
COLUMBIA

Dr. William Polk
General Surgeon
NASHVILLE

Dr. Drew Reynolds
General Surgeon
SAINT THOMAS WEST

Dr. Joshua Taylor
General Surgeon
SMYRNA

Dr. Davidson Oxley
General Surgeon
COLUMBIA

Dr. Tyson Thomas
General Surgeon
SAINT THOMAS WEST

Dr. John Valentine
General Surgeon
HENDERSONVILLE

Dr. Patrick Wolf
General Surgeon
SAINT THOMAS WOLF

