Screenings are health check-ups done by doctors to spot diseases or health problems before you have symptoms. They’re important because they catch problems early before significant issues occur and when they’re easier to treat.
Most people know about screenings such as pap smears, mammograms, prostate exams, and colonoscopies. However, vascular screenings, particularly PAD screenings, are far less discussed.
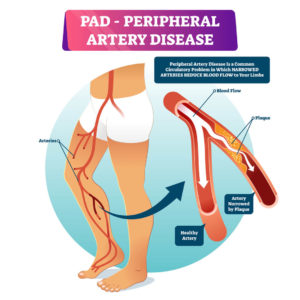
PAD, or peripheral artery disease, occurs when the arteries in your legs become narrowed or blocked, usually due to plaque buildup. This can lead to difficulties walking and, in severe cases, may result in tissue damage, infections, and even the need for amputation. PAD also places you at a higher risk of experiencing heart attacks or strokes.
Each year, the start of September marks the beginning of Peripheral Artery Disease (PAD) Awareness Month. As the name suggests, the primary aim of this month is to raise awareness about PAD and encourage individuals at risk to undergo screening for the condition.
In this blog, our goal is to do just that by providing comprehensive information about PAD. We will cover its definition, causes, symptoms, available treatment options, recommendations for screening, and the significance of PAD screening in maintaining vascular health.
WHAT IS PERIPHERAL ARTERY DISEASE?
Peripheral artery disease (PAD) is a vascular condition characterized by the narrowing or blockage of arteries, predominantly caused by atherosclerosis, a systemic disease where fatty deposits, cholesterol, and other substances accumulate inside the arterial walls, forming plaques. These plaques can harden and narrow arteries over time, restricting blood flow to various body parts.
Arteries supplying blood to the extremities, particularly the legs, are commonly affected, leading to symptoms such as leg pain, cramping, and weakness, especially during physical activity.
However, as a systemic disease, atherosclerosis affects arteries throughout the body.
The same process that causes blockages in the leg arteries can also occur in the coronary arteries supplying the heart and the carotid arteries in the neck, increasing the risk of life-threatening complications such as heart attacks and strokes. In severe cases, PAD can result in tissue damage, ulcers, and even gangrene, which may necessitate amputation if left untreated.
Recent data indicates that approximately 6.5 million people aged 40 and older in the United States are living with PAD. It affects both men and women, but certain demographic groups, such as African Americans, are at a higher risk. Hispanics may also have comparable or slightly higher rates of PAD compared to non-Hispanic white individuals.
PAD can vary in severity depending on individual factors such as overall health, lifestyle, and the presence of other medical conditions. In some cases, PAD may not cause any serious complications, while in others, it can lead to significant health risks, including limb amputation or even death if left untreated.
It’s crucial for individuals with PAD risk factors to get screened for PAD regularly. Caught early and well managed, PAD can be effectively treated, improving quality of life and reducing the risk of complications.
WHAT ARE THE SYMPTOMS OF PAD?
Symptoms of PAD can vary in presentation and severity. The primary challenge with PAD is that most people do not notice the symptoms until a critical issue arises. Additionally, symptoms resembling those of PAD can come from various other health conditions and artery disorders, and not all cases of PAD are solely attributable to atherosclerosis. This can make PAD challenging to diagnose.
That said, some signs can be detected and diagnosed with a simple screening. Recognizing these symptoms and seeking timely medical evaluation is crucial for diagnosing PAD and implementing appropriate treatment strategies to improve vascular health and quality of life.
Leg Pain (Claudication)
One of the hallmark symptoms of PAD is leg pain, particularly during physical activity like walking or climbing stairs, a condition known as claudication. Claudication arises due to inadequate blood flow to the leg muscles, depriving them of oxygen and nutrients necessary for proper function.
This pain typically occurs in the calves, thighs, or buttocks and is often described as cramping or aching. The discomfort tends to subside with rest but returns upon resuming activity.
Related: Peripheral Arterial Disease: Don’t Ignore It
Weak or Absent Pulse in Legs or Feet
In advanced stages of PAD, weakened or absent pulses in the legs and feet become noticeable. This occurs because the arteries supplying blood to the extremities have become significantly narrowed or blocked, impeding the normal flow of blood. As a result, the pulse in these areas may become weak or undetectable during a routine examination.
Ulcers, Sores, or Open Wounds
As PAD progresses, individuals may develop ulcers, sores, or open wounds on their legs or feet. Poor circulation impairs the body’s ability to heal wounds effectively, resulting in slow-healing or non-healing ulcers. These wounds may be painful, prone to infection, and require specialized wound care to facilitate healing.
Poor Toenail Growth
In some cases of advanced PAD, individuals may experience poor toenail growth due to reduced blood flow to the toes. This can manifest as thickened, brittle, or discolored toenails, indicating compromised vascular health in the affected area.
Temperature Differences
PAD can cause noticeable temperature differences between one leg and the other, with the affected limb often feeling cooler to the touch. This temperature disparity indicates impaired blood circulation and warrants further evaluation by a healthcare provider.
Hair Loss
Another potential symptom of PAD is hair loss on the legs or feet. Reduced blood flow can lead to decreased hair growth in the affected areas, resulting in sparse or absent hair follicles.
Gangrene or Tissue Decay
In severe cases of PAD, particularly when left untreated, individuals may develop gangrene or tissue decay in the affected limbs. Gangrene is characterized by tissue death due to insufficient blood supply, resulting in discoloration, necrosis, and foul odor. Prompt medical attention is essential to prevent the spread of gangrene and preserve limb function.
WHAT IS THE MAIN CAUSE OF PAD?
Peripheral artery disease (PAD) arises primarily due to atherosclerosis, a complex process characterized by the buildup of plaque within the arteries. This plaque consists of cholesterol, fatty substances, cellular waste, and other materials, gradually narrowing the arteries and impeding blood flow to vital organs and extremities.
Risk factors for atherosclerosis range from high blood pressure, high cholesterol levels, and smoking to diabetes, obesity, and a sedentary lifestyle.
While atherosclerosis is the leading cause of PAD development, several other factors contribute significantly to its onset and progression. Among these, age stands out as a prominent risk factor, with the prevalence of PAD increasing notably in individuals over the age of 50. Smoking and diabetes play a significant role in the development of PAD.
By understanding the main causes of PAD, you can take proactive steps to mitigate risk factors and prioritize vascular health.
PAD RISK FACTORS
Early detection of PAD offers a window of opportunity for prompt intervention and treatment. The earlier PAD is identified, the more manageable it becomes. That’s why understanding your risk of developing PAD is essential.
When it comes to preventing PAD, some risk factors are within your control, and others are not. If you have any of the following risk factors for peripheral artery disease, you should get screened, regardless of whether you’re experiencing symptoms.
Age
PAD can occur in younger individuals, but it becomes significantly more prevalent as people reach their 50s. By the age of 70 and beyond, the likelihood of developing PAD becomes even more pronounced. This increased risk is attributed to age-related changes in the arteries, such as the accumulation of plaque and decreased arterial flexibility.
Therefore, individuals aged 50 and above, especially those in their 60s and 70s, should be particularly vigilant about getting vascular screenings, monitoring their vascular health, and addressing any risk factors to mitigate the onset and progression of PAD.
Diabetes
Among the prominent risk factors for PAD is diabetes. Individuals with diabetes are at a significantly higher risk of developing PAD due to the impact of high blood sugar levels on blood vessels.
The UCSF Department of Surgery recommends that people aged 50 and older with diabetes undergo PAD screening to facilitate early detection and intervention.
Smoking
Smoking is another major contributor to PAD development. Tobacco smoke contains harmful chemicals that damage the arteries, leading to the formation of plaque and narrowing of blood vessels.
Quitting smoking is crucial in reducing the risk of PAD and other vascular diseases. People with a history of smoking, regardless of age, are at increased risk for PAD and should undergo a vascular screening.
Family History
A family history of PAD or related cardiovascular conditions elevates the risk of developing PAD. Individuals with relatives who have had PAD, heart disease, or strokes are more likely to develop the condition themselves.
Heart Disease, High Blood Pressure, and High Cholesterol
Other cardiovascular risk factors, including heart disease, high blood pressure, and high cholesterol levels, are closely linked to PAD. These conditions contribute to the progressive damage of arterial walls, increasing the likelihood of PAD development.
History of Stroke
A history of stroke indicates an increased risk of vascular diseases, including PAD. If you have experienced a stroke, you should be vigilant about monitoring your vascular health and addressing any modifiable risk factors to prevent further complications.
Metabolic Syndrome
Metabolic syndrome, a cluster of conditions including obesity, high blood sugar, high blood pressure, and abnormal cholesterol levels, can all significantly heighten the risk of PAD.
Managing metabolic syndrome through lifestyle modifications and medical interventions is crucial for reducing the risk of PAD and improving overall cardiovascular health.
WHY YOU SHOULD GET SCREENED FOR PAD
Peripheral artery disease (PAD) presents a significant threat to vascular health, capable of wreaking havoc if allowed to progress unchecked. The symptoms outlined earlier, ranging from leg pain to non-healing wounds, are not just signs of trouble; they indicate potentially serious problems.
Left untreated, PAD can lead to severe consequences, including the frightening prospect of limb loss and heightened susceptibility to life-threatening vascular events like heart attacks and strokes. This alone underscores the urgency of early detection through screening initiatives.
The silent progression of PAD further emphasizes the importance of proactive screening efforts. Many people with PAD may not exhibit symptoms until the disease has advanced significantly. By the time symptoms manifest, the disease may have already inflicted considerable damage.
PAD screening is critical in identifying PAD in its earliest stages when interventions are most effective and outcomes are most favorable. Early detection allows you to address PAD before it progresses. Additionally, the earlier that PAD is detected, the sooner it can be treated. Which will save you from expensive and serious medical operations down the road.
From lifestyle modifications and medication management to minimally invasive procedures and surgical interventions, early intervention provides a broader spectrum of choices for managing PAD and mitigating associated risks.
The prevalence of PAD in the United States is expected to triple in the next 30 years. But it doesn’t have to be that way. By recognizing the importance of early detection and heeding the call for screening, you can take decisive action to protect yourself against the potentially devastating consequences of untreated PAD.
Undergoing screening for PAD is not merely a precautionary measure but a proactive investment in health and well-being.
Learn more about Why PAD Matters from the American Heart Association.
WHAT IS A PAD SCREENING?
A PAD screening helps detect cardiovascular abnormalities. It is a crucial step in identifying and diagnosing peripheral artery disease (PAD), enabling early intervention to mitigate its progression and associated risks.
During a short office visit, your doctor can easily detect and diagnose PAD symptoms using various tests to assess vascular health and detect PAD symptoms effectively. PAD screening methods offer a range of options tailored to individual needs.
Here are some of the most common tests used in a PAD screening. While all these methods serve diagnostic purposes related to vascular health, they differ in terms of invasiveness, the type of information they provide, and how they are performed.
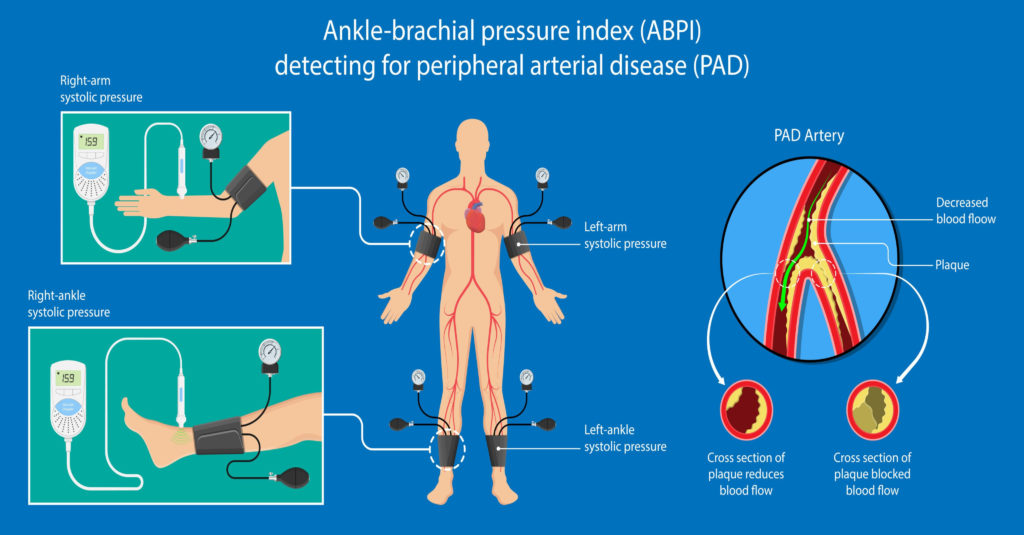
Ankle-Brachial Index (ABI)
Among the most reliable PAD screening methods is the ankle-brachial index (ABI) test. Using a handheld ultrasound device, your doctor measures blood pressure at your ankle and compares it to that of your arms. A low ABI indicates potential narrowing of veins and arteries, a hallmark of PAD.
Pulse Volume Recording
An alternative to ABI testing is pulse volume recording (PVR), which assesses changes in blood volume in your legs. Your doctor utilizes blood pressure cuffs to measure these fluctuations, providing valuable insights into vascular function.
Treadmill Test
Some screenings may include a treadmill test, during which changes in blood pressure and leg pain are monitored while walking or running. This test helps evaluate PAD symptoms under exertion, offering valuable diagnostic information.
Vascular Ultrasound
A non-invasive and stress-free test, vascular ultrasound utilizes a handheld ultrasound device to visualize blood flow through your arteries. This method provides real-time imaging of vascular structures, aiding in the detection of arterial abnormalities associated with PAD.
Intravascular Ultrasound
This ultrasound technique utilizes a catheter-mounted camera, offering a detailed examination of veins and arteries, providing valuable insights into vascular health and guiding treatment decisions.
Magnetic Resonance Angiogram (MRA)
For a comprehensive evaluation of arterial health, your doctor may recommend an MRA, an MRI-based test focusing on your circulatory system. However, due to safety concerns, individuals with certain medical devices, such as pacemakers or metal implants, may not be suitable candidates for this test.
Arteriogram
Another detailed PAD examination option is an arteriogram, which involves injecting a contrast dye into your bloodstream for X-ray imaging of your arteries. While more invasive, arteriograms provide a comprehensive “road map” of vascular health, aiding in treatment planning.
PAD TREATMENT OPTIONS
Treating PAD involves different approaches to improve blood flow, relieve symptoms, and stop the condition from worsening. At the Surgical Clinic, our providers offer various treatments to suit each person’s needs.
Here are some common options for PAD treatment:
Medication Therapy
Medications such as antiplatelet agents, statins, and blood thinners may be prescribed to manage PAD symptoms and reduce the risk of blood clots and cardiovascular events.
Lifestyle Modifications
Adopting a heart-healthy lifestyle can significantly improve PAD outcomes. This includes smoking cessation, regular exercise, a balanced diet low in saturated fats and cholesterol, and maintaining a healthy weight.
Angioplasty and Stenting
Angioplasty involves the insertion of a catheter with a balloon at its tip into the affected artery. The balloon is inflated to widen the artery and improve blood flow. In some cases, a stent may
be placed to help keep the artery open.
Vein Bypass Surgery
In cases where arterial blockages are severe or extensive, vein bypass surgery may be recommended. This procedure involves using a healthy vein from another part of the body to bypass the blocked artery, restoring blood flow to the affected area.
Trans-Carotid Artery Revascularization (TCAR)
TCAR is an innovative procedure that offers improved results and lower risks compared to traditional stenting procedures. During TCAR, a small incision is made at the base of the neck to access the carotid artery, allowing for the precise placement of a stent to improve blood flow.
Exercise Rehabilitation Programs
Supervised exercise programs, such as cardiac rehabilitation, can help improve PAD symptoms, increase walking distance, and enhance overall cardiovascular fitness.
Wound Care and Limb Salvage
For individuals with PAD-related wounds or ulcers, specialized wound care techniques may be employed to promote healing and prevent complications such as infection or limb loss.
Amputation Prevention
In advanced cases of PAD where limb-threatening ischemia is present, interventions such as endovascular revascularization or surgical bypass may be necessary to preserve limb function and prevent amputation.
PREVENTING OR MANAGING PAD
Depending on your symptoms, health, and medical history, you may be able to take proactive steps to reduce your risk of PAD. If you’ve already been diagnosed with PAD, there are effective steps you can take to manage it before complications arise.
Preventing or managing PAD involves a combination of lifestyle changes, healthy habits, and medical interventions tailored to individual needs. Here are some strategies to consider:
Regular Check-ups and Vascular Screenings
Schedule regular check-ups with your healthcare provider to monitor your vascular health, assess risk factors for PAD, and discuss preventive measures and treatment options.
Quit Smoking
Smoking is a major risk factor for PAD. Quitting smoking can significantly reduce your risk of developing PAD and improve overall cardiovascular health.
Healthy Eating
Adopting a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help lower cholesterol levels, maintain a healthy weight, and reduce the risk of PAD.
Regular Exercise
Regular physical activity, such as walking, swimming, or cycling, can improve circulation, strengthen veins, and reduce the risk of PAD. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Manage Chronic Conditions
Proper management of underlying health conditions such as diabetes, high blood pressure, and high cholesterol is essential for preventing PAD and reducing its progression. Follow your healthcare provider’s recommendations for medication management, regular check-ups, and monitoring of these conditions.
Maintain a Healthy Weight
Excess weight puts added strain on the circulatory system and increases the risk of developing PAD. Aim to achieve and maintain a healthy weight through a combination of diet and exercise.
Control Blood Sugar Levels
If you have diabetes, it’s essential to monitor and control your blood sugar levels to prevent complications such as PAD. Follow your healthcare provider’s recommendations for medication management, blood sugar monitoring, and lifestyle modifications.
Foot Care
If you have PAD, proper foot care is essential to prevent complications such as ulcers and infections. Inspect your feet regularly for any signs of injury or infection, and seek prompt medical attention for any foot-related concerns.
PAD TREATMENT AT THE SURGICAL CLINIC IN TENNESSEE
At The Surgical Clinic, we have many surgeons and medical providers trained in vascular health and vascular surgery. If you or a loved one are at risk for PAD, give us a call to schedule an appointment. Don’t wait for an emergency. Be proactive about your vascular health.

