Bariatric surgery is a key medical intervention for those grappling with severe obesity, especially when diet and exercise have proven ineffective. By modifying the digestive system, bariatric surgery helps achieve significant weight loss and improves obesity-related health conditions. In this article, you’ll learn about the types of bariatric surgery, who it suits best, and what results you can anticipate.
Main Points
- Bariatric surgery offers significant, long-term weight loss and improvement in obesity-related health conditions by modifying the digestive system, with procedures like gastric bypass and sleeve gastrectomy being highly effective.
- Recognizing obesity as a chronic disease influenced by genetic factors can reduce stigma and foster a supportive healthcare environment, essential for successful weight management and treatment.
- Determining candidacy for bariatric surgery involves evaluating BMI, medical conditions, and co-morbidities, with long-term success requiring substantial lifestyle changes, dietary adjustments, and regular follow-ups.
Understanding Bariatric Surgery
Bariatric surgery is a powerful tool in the fight against severe obesity, involving surgical changes to the digestive system to promote weight loss. It’s typically recommended when traditional methods like diet and exercise have failed, or when serious health issues arise due to obesity. The transformative impact of metabolic and bariatric surgery is undeniable, often resulting in sustainable weight loss and remarkable improvements in obesity-related health conditions.
There are various bariatric surgery procedures, each designed to either limit food intake, reduce the body’s ability to absorb nutrients, or both. These procedures are not just about losing weight; they play a crucial role in treating obesity and its related diseases, providing a lifeline for many who struggle with severe obesity.
What is Bariatric Surgery?
Bariatric surgery is more than a weight loss surgery; it serves as a holistic treatment for severe obesity and its comorbidities. The primary goal is significant weight loss and a reduction in the risk of weight-related health complications. This surgical intervention involves altering the anatomy of the stomach and sometimes the intestines, to limit the amount of food consumed and absorbed. Some common types of bariatric surgery include:
- Gastric bypass
- Sleeve gastrectomy
- Adjustable gastric banding
- Biliopancreatic diversion with duodenal switch
These procedures can help patients lose weight, achieve long-term weight loss, and improve their overall health.
The potency of these bariatric procedures stems from their capacity to trigger significant and long-term weight loss, which subsequently leads to improvements in obesity-related conditions such as type 2 diabetes and hypertension. Patients frequently witness a reversal of these conditions, with many reporting better management of their diabetes and high blood pressure post-surgery.
Bariatric surgery is recognized by the National Institutes of Health as a highly effective treatment for long-term weight loss in severely obese individuals. Studies reveal that most bariatric surgery patients maintain an excess body mass loss of between 51% and 54% ten years after surgery. Typically performed laparoscopically, these procedures are associated with lower morbidity and mortality rates, making them a safer option for many.
Types of Bariatric Surgery
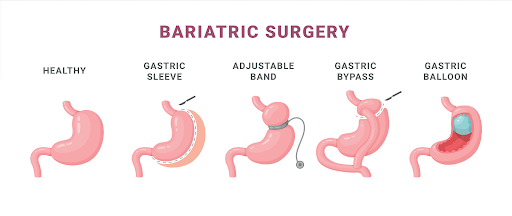
Among the commonly performed bariatric surgery procedures, sleeve gastrectomy, Roux-en-Y gastric bypass, and gastric band stand out due to their effectiveness and longevity.
The sleeve gastrectomy involves removing a large portion of the stomach, leaving a tube-like structure or “sleeve.” This notably restricts the amount of food the patient can consume, assisting with weight loss.
The Roux-en-Y gastric bypass, often referred to as gastric bypass surgery, is another highly effective procedure. This procedure entails:
- Creating a small pouch out of the upper stomach that is directly connected to the small intestine
- Bypassing a large part of the stomach and duodenum
- Limiting food intake
- Reducing nutrient absorption
- Resulting in significant and lasting weight loss.
Both these bariatric procedures offer a mortality benefit and a decrease in medical comorbidities. They are often performed using minimally invasive techniques like laparoscopic surgery, which reduces recovery time and the risk of complications.
Patients who undergo bariatric surgery usually embark on a journey towards a healthier, more active lifestyle, liberated from the constraints of severe obesity.
Addressing Stigma and Supporting Patients
In the realm of healthcare, addressing the stigma surrounding obesity is as crucial as the medical treatment itself. Even in healthcare settings, patients with obesity frequently encounter judgment and prejudice, which can significantly impact their willingness to seek help. Healthcare practitioners play a pivotal role in combating this stigma, fostering a non-judgmental and supportive environment that encourages patients to pursue obesity treatment without fear of discrimination.
Short consultation times and perceived lack of motivation from the patient are common barriers practitioners face when discussing obesity. Yet, acknowledging obesity as a chronic disease, rather than an unhealthy lifestyle consequence, can aid in altering this perspective. This not only improves patient outcomes but also promotes a more empathetic approach to treating obesity.
Recognizing Obesity as a Disease
Obesity is increasingly recognized as a chronic and genetic disease, necessitating a shift in how healthcare practitioners approach its treatment. With up to 70% of obesity attributed to genetic factors, it’s crucial for practitioners to understand the complex interplay of genetics and environment in their patients’ weight issues. This recognition aligns with international guidelines and underscores the need for comprehensive, multifaceted treatment strategies.
Understanding obesity as a genetic disease, influenced by numerous genes and environmental factors, helps dispel the myth that it’s purely a result of lifestyle choices. This change in viewpoint cultivates a more empathetic methodology towards weight loss surgery and other obesity treatments, emphasizing that losing weight is not merely a matter of willpower but involves addressing underlying medical conditions.
Providing Encouragement
Encouraging patients with obesity in a supportive and non-judgmental manner is essential for successful weight management. Patients frequently articulate their need for guidance and support from their healthcare providers, and a compassionate approach can make a significant difference in their journey. Blaming patients for their weight issues only exacerbates feelings of personal failure and discourages them from seeking help.
Healthcare providers should focus on creating an environment where patients feel heard and supported. By offering encouragement and practical advice, providers can help patients navigate the challenges of losing weight and maintaining a healthy lifestyle. This supportive approach is crucial for the long-term success of bariatric surgery patients, who rely on continual guidance to achieve their health goals.
Candidacy for Bariatric Surgery
Determining candidacy for bariatric surgery, or a weight loss surgery, involves a comprehensive evaluation process. Candidates must meet specific Body Mass Index (BMI) requirements and have a documented history of weight management attempts. This guarantees that surgery is only contemplated after other weight loss methods have been attempted and found to be unsuccessful.
In addition to BMI criteria, candidates undergo thorough evaluations for medical conditions and comorbidities. A multidisciplinary team of medical, surgical, psychiatric, and nutritional experts assesses each patient to ensure they are suitable candidates for bariatric surgery. This stringent screening process aids in identifying potential risks and guarantees that patients are adequately prepared for the surgery and the subsequent lifestyle changes. Let’s look at some key weight loss surgery requirements below.
Body Mass Index (BMI) Requirements
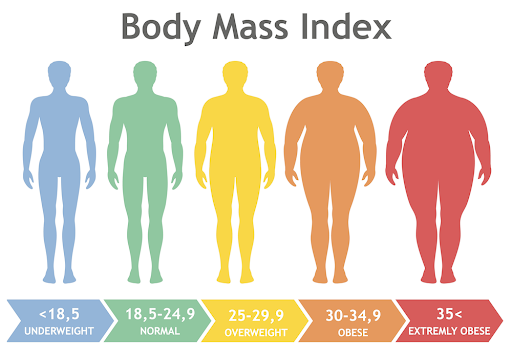
Body Mass Index (BMI) is a crucial factor in determining eligibility for bariatric surgery. Typically, surgery is considered for individuals with a BMI of 40 or higher, which indicates severe obesity. For those with a BMI between 35 and 40, related health conditions such as sleep apnea, high blood pressure, heart disease, or type 2 diabetes are also considered. These conditions often exacerbate the health risks associated with obesity, making surgical intervention more urgent.
In some cases, individuals with a BMI of 30-34.9 may be considered for surgery if they have serious metabolic diseases and have not achieved desired weight loss with non-surgical methods. This flexibility in BMI requirements allows for a tailored approach, ensuring that those who need the surgery most can access it.
Medical Conditions and Comorbidities
When determining candidacy for bariatric surgery, healthcare providers also consider the presence of medical conditions and co-morbidities related to excess weight. Conditions like type 2 diabetes, obstructive sleep apnea, and high blood pressure play a significant role in this evaluation. These obesity-related conditions not only impact overall health but also increase the urgency for effective weight loss solutions.
However, patients with advanced heart or lung disease may not be suitable candidates for surgery due to the increased risk of complications.
Long-term Effects and Maintenance
Achieving long-term success post-bariatric surgery necessitates considerable lifestyle modifications and continuous medical care. Patients must commit to a lifetime of dietary adjustments, regular follow-ups, and monitoring to maintain their weight loss and overall health. While the surgery itself provides a powerful tool for weight loss, its effectiveness is maximized through diligent post-operative care and lifestyle modifications.
Potential complications can arise, with around 20% of patients experiencing issues such as food intolerance, weight regain, and relationship problems. Weight regain typically starts in the third year post-surgery and can be influenced by factors such as the size of the stomach sleeve or failure to adhere to recommended lifestyle changes. Comprehending and managing these complications is vital for guaranteeing long-term success.
Dietary Changes

Post-surgery dietary changes are pivotal for maintaining weight loss and preventing complications. Patients are generally advised to follow a calorie-restricted diet, consuming between 1000 to 1400 calories per day, with a focus on high-protein foods. Protein intake should be around 60 to 80 grams daily to preserve muscle tissue.
To minimize the risk of complications related to digestive and kidney diseases, certain foods like sugary and starchy items, as well as habits like alcohol consumption and smoking, should be reduced or stopped altogether. Patients may also experience food intolerance issues, particularly with items like red meat, rice, pasta, and bread.
Two weeks after surgery, a diet of blended and puréed high-protein, low-calorie foods can be introduced. Lifelong vitamin and mineral supplementation is essential to address potential nutritional deficiencies.
Regular Follow-ups
Frequent follow-ups with healthcare providers are vital for tracking progress and handling any complications that may surface post-surgery. These appointments help ensure that patients adhere to dietary guidelines and adjust medication plans as needed. Long-term medical follow-up is necessary to maintain health outcomes and prevent issues such as malnutrition and gastroesophageal reflux disease (GERD).
Patients are advised to contact their healthcare provider if they experience symptoms like fever, difficulty breathing, chest pain, or persistent vomiting. Regular follow-ups also help in managing conditions like dumping syndrome, which can cause nausea, rapid heartbeat, and abdominal pain. Lifelong vitamin and mineral supplementation, such as calcium and vitamin D, is also necessary to prevent deficiencies and maintain overall health.
Summary
Bariatric surgery offers a transformative solution for those struggling with severe obesity. From understanding the different types of procedures to recognizing the importance of addressing stigma and providing support, this guide has covered the essential aspects of bariatric surgery. The candidacy requirements, long-term effects, and necessary lifestyle changes highlight the commitment required for success. By embracing this life-changing intervention, patients can achieve significant weight loss, improved health outcomes, and a renewed sense of hope. Let this be the beginning of a healthier, happier you.
Frequently Asked Questions
What is bariatric surgery?
Bariatric surgery is a surgical intervention for severe obesity that alters the digestive system to achieve significant weight loss.
Who is a candidate for bariatric surgery?
Candidates for bariatric surgery typically have a BMI of 40 or higher, or between 35 and 40 with obesity-related health conditions such as type 2 diabetes or sleep apnea. This surgery is considered for those with severe obesity or related health conditions.
What are the common types of bariatric surgery?
The most common types of bariatric surgery are sleeve gastrectomy and Roux-en-Y gastric bypass, both of which lead to significant and lasting weight loss.
What dietary changes are required after bariatric surgery?
After bariatric surgery, it’s important to follow a calorie-restricted, high-protein diet and avoid certain foods to lower the risk of complications.
Why are regular follow-ups important after bariatric surgery?
Regular follow-ups after bariatric surgery are important for monitoring health, managing complications, and adjusting dietary or medication plans to ensure long-term success. They help ensure the best possible outcomes and support your overall well-being.

